Extensive macular atrophy with pseudodrusen-like appearance (EMAP), a fairly new diagnosis, is an aggressive form of adult-onset macular atrophy characterized by the funduscopic triad of macular atrophy with major vertical axis, mid-peripheral pseudodrusen-like lesions and peripheral retinal degeneration. In EMAP, macular atrophy begins superior to the fovea and rapidly grows on the vertical axis. Foveal involvement occurs within four years, leading to severe visual loss, although no survival analysis has been performed to date.
EMAP, first described in 2009, remains an underrecognized condition, especially among the elderly, who are more likely to be misdiagnosed with AMD. This is particularly true for patients that seek the advice of a retina specialist in their 60s or later, after the established 55-year-old cut-off, and for those who cannot recall the earliest onset of their symptoms.
 |
|
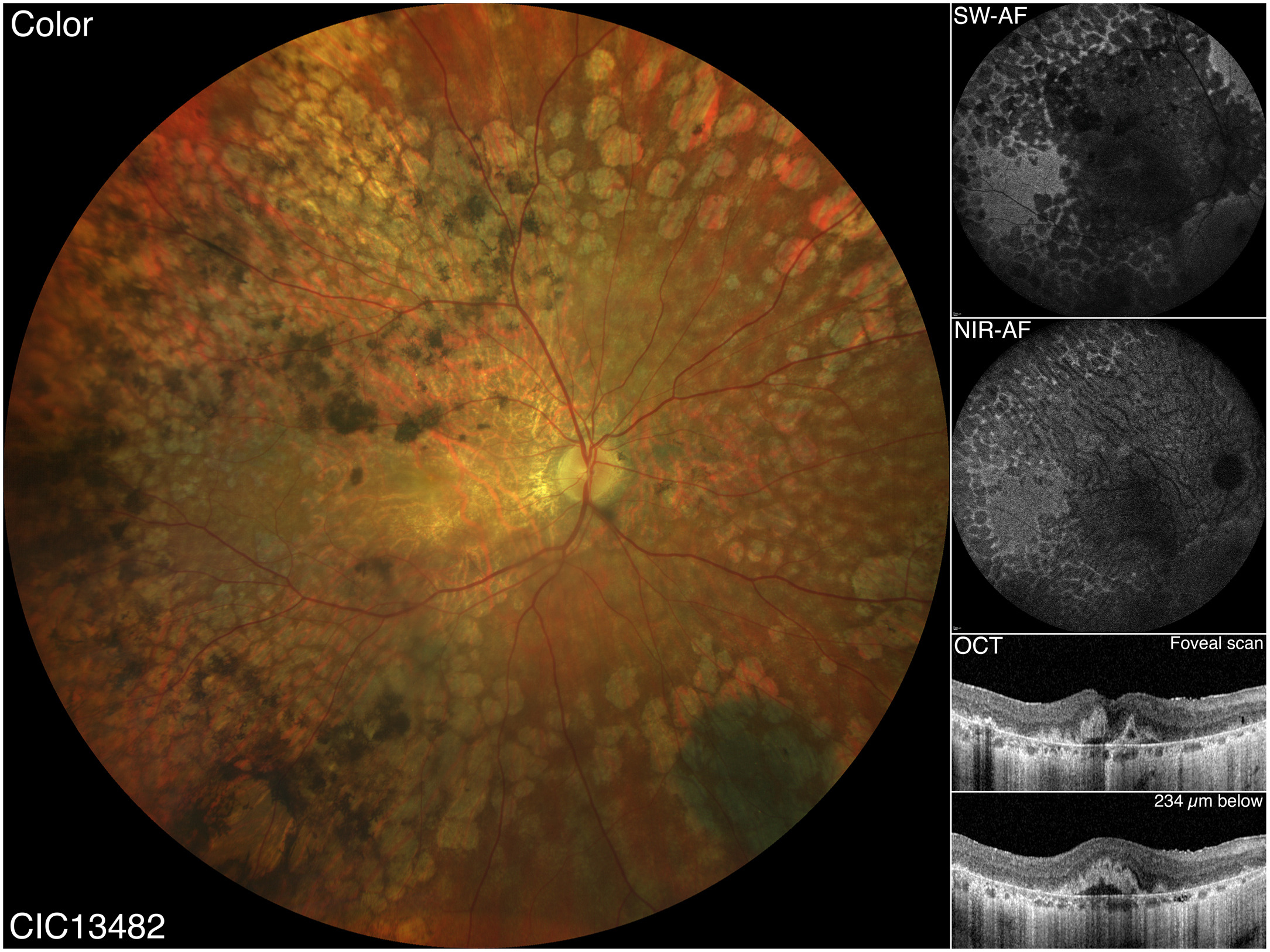
EMAP remains an underrecognized condition, especially among the elderly, who are more likely to be misdiagnosed with AMD. Earlier onset, more rapid progression of atrophy, and severe visual loss were noted in the former in contrast to the latter condition. The multimodal imaging of advanced EMAP above (from the study) exhibits a diffuse retinal involvement with “confluent” pavingstone-like degeneration merging with the extensive macular atrophy. OCT reveals large hyperreflective pyramidal structures within the atrophic fovea that are not clearly visible on color fundus photograph. Photo: Antropoli A, et al. Ophthalmol. April 5, 2024. Click image to enlarge. |
Researchers in Paris recently described the clinical outcome and late-stage findings of EMAP in a large, elderly cohort. Based on our survival analyses, they found that BCVA in EMAP frequently remained above the WHO blindness threshold or took several years to reach it. These patients were unaffected by age of onset, and the study, which was published in Ophthalmology, has emphasized the need of proper phenotyping for correctly diagnosing EMAP even in patients outside the conventional age range.
From 78 patients (156 eyes) affected by EMAP, the research team collected data on BCVA, kinetic perimetry, OCT, short-wavelength autofluorescence and near-infrared autofluorescence. At the most recent visit, the mean age was 70.9.
The study calculated incidence rates for blindness and different atrophy checkpoints. These patients experience severe visual impairment beyond visual acuity decline, with large central scotomas and, eventually, peripheral visual field constriction. The researchers found that 58.1% of the patients were blind with the US criteria, and 25.8% according to the WHO. Vision of 20/200 or worse was typically attained after about four years, aligning with the median time before foveal atrophy occurs (3.4 years). Subsequently, the atrophy extended beyond the central 30° within 4.7 years, and beyond the mid-periphery after seven years or later. In EMAP, the atrophy initially grew vertically rather than enlarging in a strictly centrifugal pattern, before radiating towards the periphery. The researchers detected focal openings or large dehiscences of the Bruch’s membrane in 25.4% of the eyes.
Near-infrared autofluorescence showed increased visibility of the choroidal vessels beyond the atrophy in 87.2% of the eyes. Using this imaging modality to enhance focus on retinal pigment epithelium (RPE) and melanin, the researchers found an increased visibility of the choroidal texture beyond the atrophic area in over 80% of the cases. The study proposed that this phenomenon could reflect a diffuse RPE sufferance because of the toxic effect of the sub-RPE deposits or the longstanding separation from Bruch’s membrane.
“The visual acuity plateau experienced by our patients might be linked to the development of an eccentric preferred retinal locus in adjacent preserved areas, like in AMD or Stargardt disease,” the researchers wrote in their paper. “Our analyses revealed that the age at which a patient first experiences symptoms or receives a diagnosis does not significantly influence the risk of atrophy involving the fovea or expanding beyond the central 30° and 55°.”
“Our imaging findings suggest a primary role of the RPE-Bruch’s membrane complex in the pathogenesis of the disease,” they concluded. “Our findings expand the knowledge on one of the most aggressive retinal diseases and provide insights regarding its progression kinetics and visual outcomes.”
Antropoli A, Biano L, Condroyer C, et al. Extensive macular atrophy with pseudodrusen-like appearance (EMAP): progression kinetics and late-stage findings. Ophthalmology. April 5, 2024. [Epub ahead of print]. |


