As one of the more perplexing diseases optometrists handle on a daily basis, glaucoma presents with a variety of vascular and retinal abnormalities. While the pathophysiology of the progressive condition remains indefinite, newer technologies such as OCT-A offer better visualization of its clinical manifestations. Polygenic risk scores (PRS) have also proven useful in recent years to determine patient risk of glaucoma and related conditions, such as cardiovascular disease. When combining these tools to evaluate glaucoma patients or suspects, which parallels can be drawn between retinal vasculature and risk scores? Does a higher score correlate to a higher risk of retinal vascular defects?
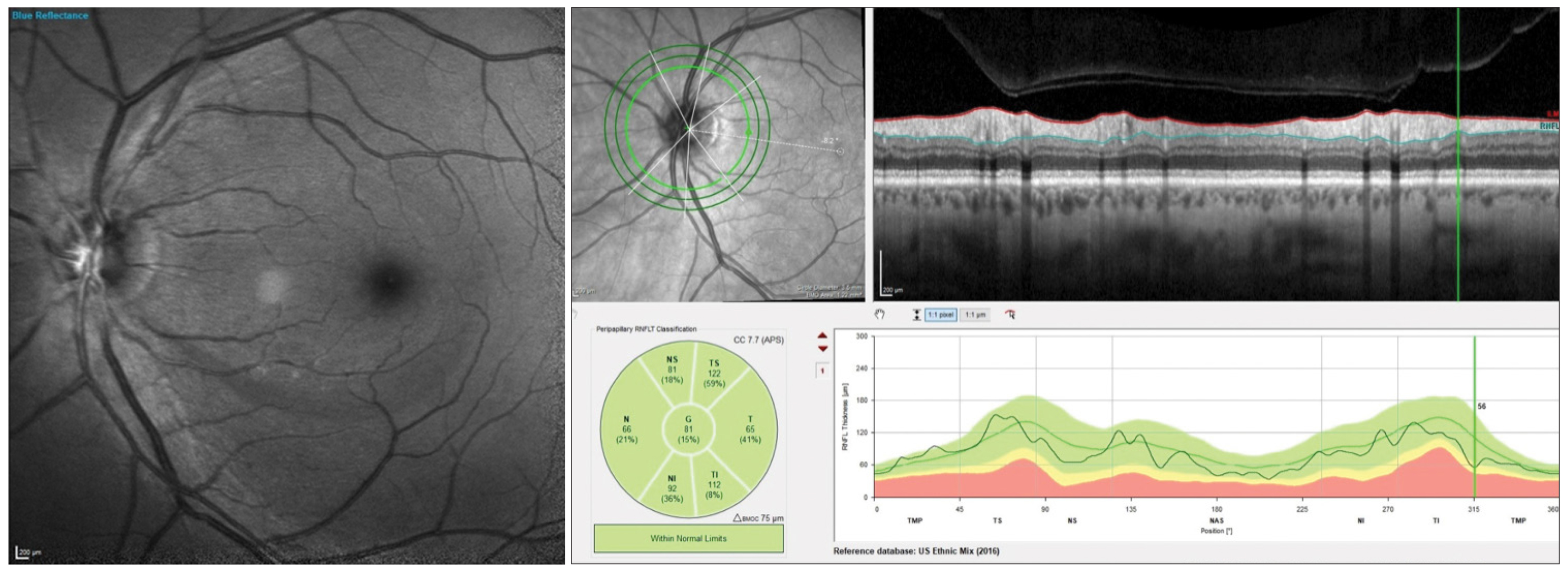 |
| Researchers found no association between vascular and RNFL wedges and systemic cardiovascular PRS, though the two findings did relate to glaucoma risk score, suggesting that vascular dropout could be a locally driven process. Photo: James Fanelli, OD. Click image to enlarge. |
To help answer these questions, researchers recently analyzed localized vascular and RNFL wedge-shaped defects on OCT-A alongside PRS for each glaucoma and cardiovascular disease. The study involved 858 eyes of 455 individuals (94% Caucasian) with suspect and early manifest primary open-angle glaucoma. They concluded that patients with a higher genetic risk of glaucoma (based on PRS) were more likely to have retinal vascular defects and structural glaucomatous loss; however, this did not relate to systemic cardiovascular risk.
The team reported that a higher PRS score was associated with the presence of multiple vascular wedges per eye. Additionally, glaucoma progression (measured based on global RNFL loss) was associated with vascular and RNFL wedge defects, which were distributed equally in 162 eyes. The data also showed that after controlling for disc hemorrhage, glaucoma PRS was significantly associated with vascular wedge defects, but not with RNFL wedge defects. On the contrary, cardiovascular genetic risk didn’t appear to share an association with vascular wedge defects.
The researchers theorized that the lack of an association between vascular and RNFL wedges and systemic cardiovascular PRS suggests vascular dropout could be a locally driven process. “It could still be that vascular dropout is secondary to the RNFL loss, but these findings may support the existence of a vascular glaucoma phenotype in some cases, while others manifest RNFL loss with no change in vasculature,” they wrote in their paper, published recently in Acta Ophthalmologica.
When evaluating eyes with vascular wedge defects, the researchers determined that these patients “were statistically more likely to be older, with lower IOP, higher vertical cup/disc ratio, lower central corneal thickness, worse visual acuity, more myopic, with worse mean deviation, greater history of disc hemorrhage and were more likely to be treated for glaucoma.” They pointed out, “These are consistent with known risks or features of glaucoma, except for the lower IOP.” All these findings also described patients with RNFL wedge defects with the exception of increased myopia severity.
Reflecting on how this data might aid in clinical practice, the researchers wrote, “The glaucoma PRS has been shown to aid in identifying individuals who are likely to develop progressive glaucoma, and this study indicates that those individuals may be more likely to present with a vascular phenotype. Identifying this predisposition early may influence treatment and clinical decisions and demonstrates a potential advantage of incorporating OCTA monitoring into clinical care,” they concluded.
Saks DG, Schulz A, Qassim A, et al. Genetic risk of glaucoma is associated with vascular and retinal nerve fibre wedge defects. Acta Ophthalmologica. October 6, 2023. [Epub ahead of print]. |

