 |
|
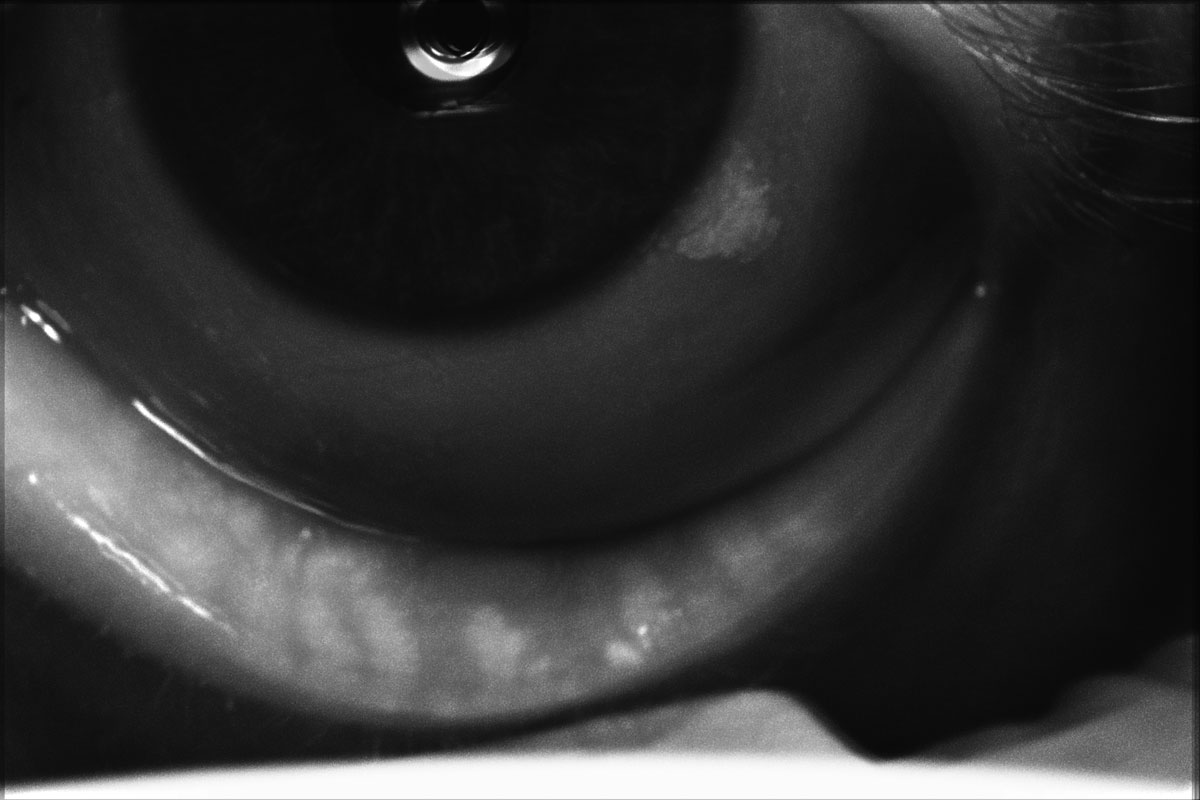
Meibography of a patient with severe dry eye disease. Note they have moderate atrophy of the glands with moderate truncation and loss of gland structure. Photo: Cecelia Koetting, OD. Click image to enlarge. |
Dry eye is quite common in patients over age 50, so it’s no surprise that the condition is pervasive in those of cataract age; ideally, it should be managed in concert with the surgical plan for the best possible outcomes. A new study funded by Johnson & Johnson Vision, makers of the LipiScan device for meibography, shows the role this technique can play in assessing cataract patients prior to surgery. Meibography offers direct observation of meibomian gland (MG) morphological architecture, independent of function, and has been shown to be useful in evaluating MG changes in MG dysfunction (MGD). Although it is less commonly measured, some researchers have used structural data to determine MGD prevalence. In the study, published in Cornea, the team found that 95% of patients presenting for cataract surgery have some evidence of MG atrophy.
Records of 391 patients aged 50 years or older who had undergone a preoperative cataract surgery workup with meibography were included. The amount of atrophy in the lower eyelid was graded on a 0-3 scale, where 0=no atrophy, 1=1-33% atrophy, 2=34-66% atrophy and 3=66% or more atrophy. Associations between MG atrophy and demography, comorbidities and risk factors were evaluated.
Functional changes in MGD typically precede structural alterations to the gland architecture. However, the percentage of patients with MG atrophy (93.2%) was significantly higher than the percentage of patients with moderate/difficult meibum expressibility or meibum quality (grade 2) (75.4%), indicating that nearly 18% of patients with cataract had structural changes despite minimal or no functional changes.
“This may suggest that structural changes to the glands sometimes precede functional alterations to meibum quality and expressibility,” the authors explained in their paper. “Alternatively, it may be that some older patients have age-related changes of the MGs resulting from a different mechanism than the commonly accepted mechanisms of ductal occlusion and hyperkeratinization.”
These findings also indicate that MGD with true MG structural changes would have been missed in some patients with good MG function had meibography not been performed, the authors suggest. Therefore, it is important to assess the meibomian glands in all patients with cataract, not just those with severe symptoms or poor MG function, the study authors argue. In addition to meibography, the glands can be evaluated at the slit lamp via transillumination.
“Treating these patients may help slow the progression of MGD and prevent chronic symptoms because symptoms have been shown to worsen with cataract surgery alone in patients with known preexisting MGD,” the authors explained. “Optimizing ocular surface health before surgery and setting patient expectations to a realistic level can prevent postoperative dissatisfaction.”
Lastly, this study showed that although severe (grade 3) atrophy was more likely in patients with a dry eye disease (DED) diagnosis, the overall rate of gland atrophy (grade 1) was similar whether previously diagnosed with it or not. “More importantly, among patients with no previous history of DED diagnosis, 18% had moderate and 13% had severe MG atrophy.”
The authors concluded that routine evaluation of gland structure during preoperative screening in cataract surgery patients, in addition to assessment of gland function, may facilitate the timely and effective diagnosis and treatment of MGD, leading to better surgical decision-making.
Yeu E, Koetting C, Calvelli H. Prevalence of meibomian gland atrophy in patients undergoing cataract surgery. Cornea. November 20, 2022. [Epub ahead of print]. |

