 |
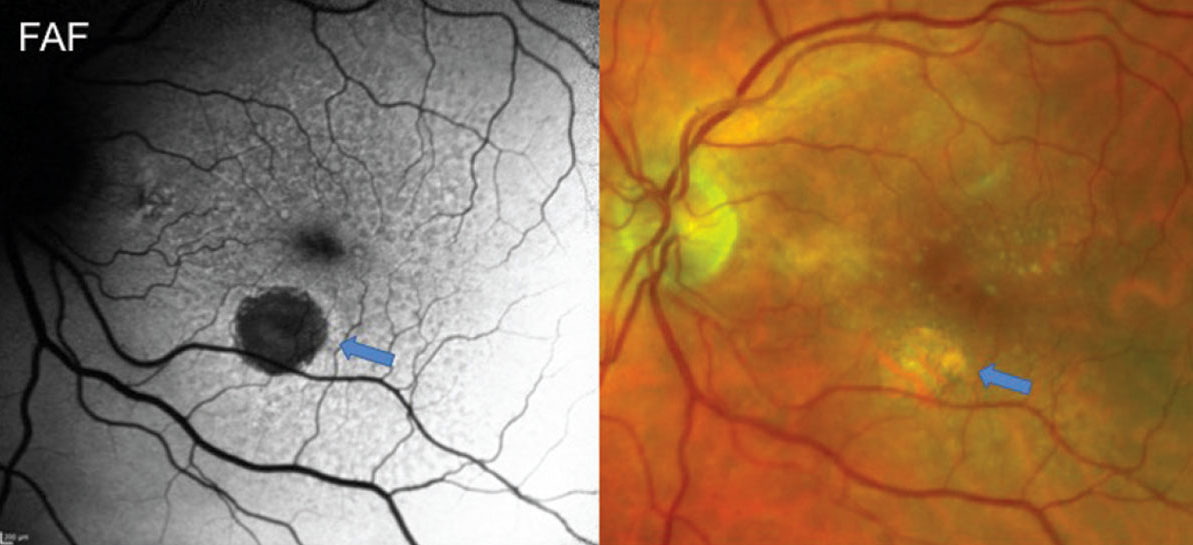
Geographic atrophy can cause meaningful disease burden by visual acuity, conversion to wet AMD and central subfield thickness measures. Photo: Jessica Haynes, OD. Click image to enlarge. |
This afternoon at ARVO 2023 in New Orleans, one study to be presented will help to characterize the extent of disease burden associated with geographic atrophy (GA). Specifically, the authors’ intention was to see how visual acuity changes and conversion to neovascular AMD (nAMD) affect geographic atrophy patients. Although geographic atrophy due to AMD is a common vision loss cause, the study authors noted that there are not many large clinical outcome studies assessing the relationship between the two.
The retrospective study included patients who were diagnosed with dry AMD with advanced atrophy. However, these patients also had to have not been diagnosed with nAMD prior to geographic atrophy diagnosis in at least one eye. A follow-up of at least three years ensued.
Baseline age was 79 years on average and 66% of patients were women. Of the 18,712 geographic atrophy eyes included, 25% were diagnosed with nAMD on average 24.7 months later. Rates of conversion by year were as follows (percentage of all GA eyes):
- within year one: 8.8%
- within year two: 5.9%
- within year three: 4.6%
- beyond year three: 6.3%
The 75% who did not develop nAMD (11,125 eyes) and still had valid visual acuity readings throughout all follow-up possessed average VA measures of 59.5 letters at baseline and a 3.1 letter loss at one year. Loss of 6.4 letters at year two was observed in 9,725 geographic atrophy eyes, and 8,870 eyes saw a 10.1 letter loss at year three.
Baseline visual acuity of less than 20/40 to 20/100 was determined to have eye loss more letters than others. Even further, eyes with geographic atrophy but with good visual acuity presented at baseline ended up losing more letters than those with worse visual acuity.
The authors make the conclusions that “those geographic atrophy eyes with modest visual acuity impairment at baseline may be at the greatest risk of further vision loss, likely from progression to subfoveal geographic atrophy. Eyes with geographic atrophy are also at meaningful risk of nAMD.” This information may help clinicians when looking at these patients.
Original abstract content © Association for Research in Vision and Ophthalmology 2023.
Ciulla TA, Boucher N, Aggarwal N, Harris A. Geographic atrophy is associated with meaningful disease burden: visual acuity changes and conversion to neovascular AMD over 3 years in 18,712 patient eyes. ARVO 2023 annual meeting. |


