 |
|
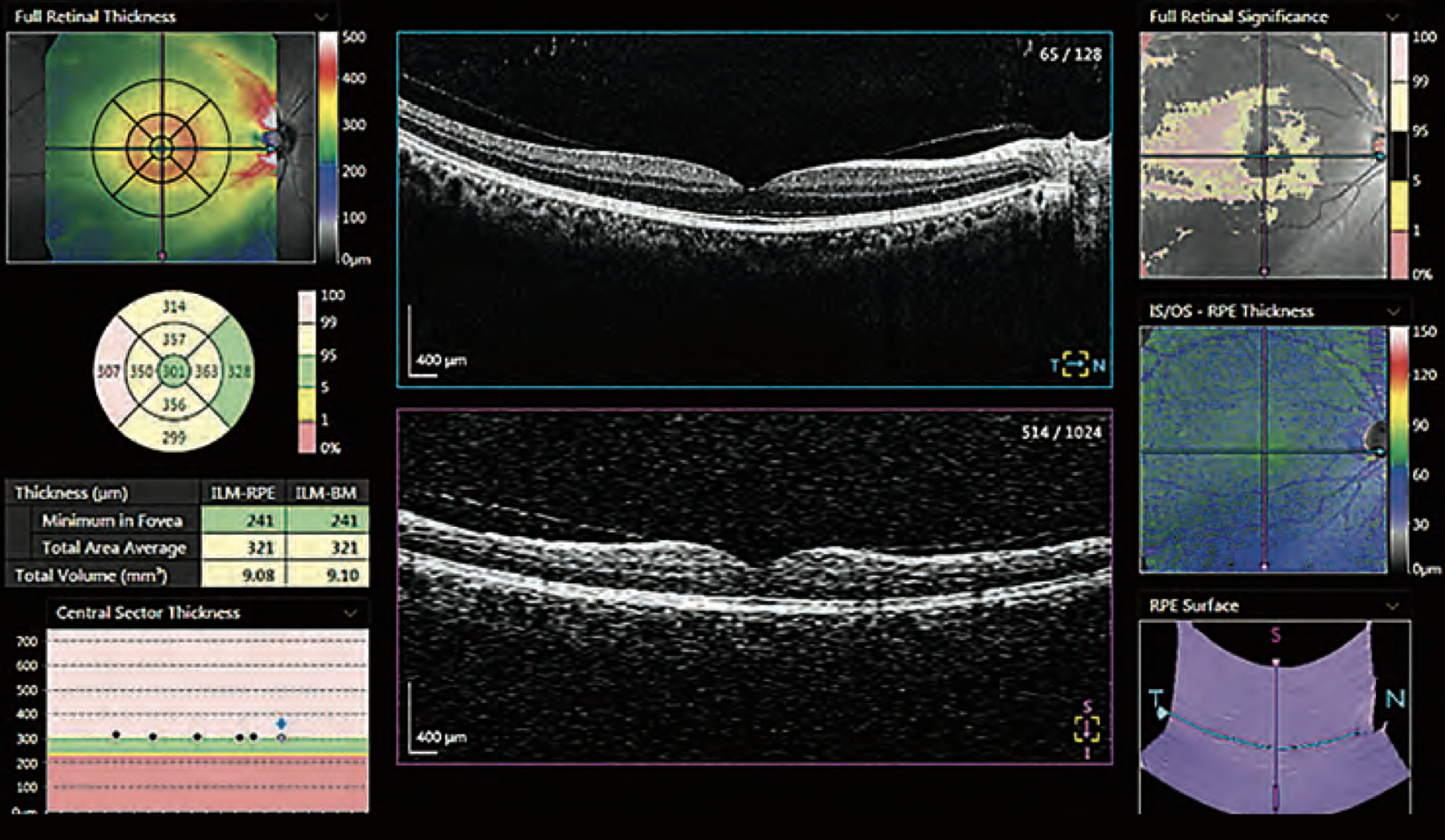
This study identified a few advantages of using total retinal thickness over RNFLT for detecting glaucoma. Photo: Canon. Click image to enlarge. |
While OCT is an invaluable tool for assessing glaucoma, one new study further delineates just how useful the technology can be. The study focused on how layer thickness assessed by different algorithms can be affected by image quality, the stage of disease, how reproducible the algorithms are and whether the algorithms agree or disagree. Subsequently, the usefulness of OCT is largely dependent on image quality used, disease stage and segmentation algorithm.
To compare measurements of retinal nerve fiber layer thickness (RNFLT) and total retinal thickness (TRT), the researchers collected optic disc OCT data from 20 healthy subjects, 28 early-stage glaucoma patients, 29 moderate and 23 severe. Four different algorithms were used in assessment. All documented that nerve fiber thickness was more sensitive to an image’s quality than was total retinal thickness. However, both factors for all four algorithms displayed noticeable differences between healthy individuals and glaucomatous patients from all categories, as well as between early and moderate stage glaucoma. Neither factor could distinguish between moderate and severe forms of glaucoma, though. The agreement between algorithms ranged from moderate to excellent.
As the researchers point out, OCT thickness layer measurements are influenced heavily by noise and the stage of glaucoma seen. RNFLT was consistently more sensitive to the quality of the image than TRT was, regardless of what algorithm was used.
Higher RNFL measurements are more commonly associated with a better-quality image, as well as displaying better thickness layer agreement when looking between scans of images of comparable quality. Conversely, there is a seeming decrease of RNFLT reported to be caused by low-quality images, and this applies both theoretically and experimentally in the macular area, around the ONH and due to cataract.
After the nerve fiber layer thins to a certain point, there is a minimum value in which further thinning progression cannot be measured by OCT—the so-called “floor effect”—thus explaining why the researchers could not find significant differences between moderate and severe types for any of the used algorithms.
Since TRT was less sensitive to image quality, the researchers believe it to be just as usable as a measurement tool as RNFLT to detect early glaucomatous damage. This is because of its greater resistance to influence of noise than RNFLT. Despite this advantage, both measurement types perform similarly in end-stage glaucoma, evidenced by reaching the floor effect.
The authors acknowledge that “the use of TRT does not solve one of the major drawbacks of OCT in clinical glaucoma care, the floor effect.” Although this disadvantage has yet to be overcome, the importance of using TRT lies within it showing “a better within and between algorithms ICC in all comparisons. Therefore, it seems worthwhile to further explore its value, especially also in longitudinal data.” Specifically, the authors hold it a more informative option when dealing with poor image quality.
Heikka T, Jansonius NM. Influence of signal-to-noise ratio, glaucoma stage and segmentation algorithm on OCT usability for quantifying layer thickness in the peripapillary retina. Acta Ophthalmol. 2022. [Epub ahead of print]. |


