 |
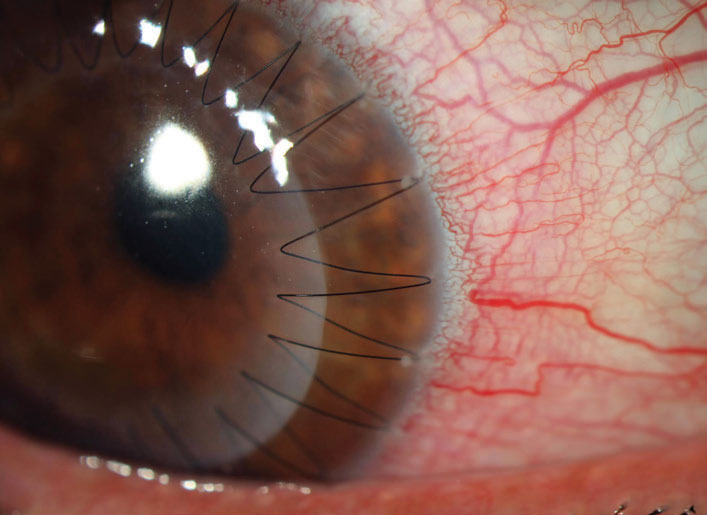
Onset of late ectasia is usually decades following PK. Photo: Aaron Bronner, OD. Click image to enlarge. |
The subtype of ectatic disease following penetrating keratoplasty (PK) has been defined poorly in the literature, with the terminology not being consistent. In contrast to Scheimpflug tomography, measurements with anterior segment optical coherence tomography AS-OCT are also possible in corneas with opacity. A research team based in Germany has used this imaging modality to describe morphological parameters of ectatic corneas after PK. They noted an acute graft-host interface angle, steep keratometry value, deep AC and a stromal thinning at the interface as significant signs of ectasia. A ratio calculated by the relationship between the thinnest point at the interface and the central corneal thickness was significantly lower in ectatic eyes.
The team included 50 eyes of 32 patients with a history of PK at an average of 25 years earlier were included, 35 ectatic and 15 not. Mean age at time of examination was 63, mean interval between PK and time of AS-OCT examination was 25 years. PK had been performed at an average age of 38. The control group consisted of 30 healthy age-matched eyes (mean age: 62). They assessed steep and flat keratometry readings obtained with AS-OCT (CASIA-2, Tomey) and Scheimpflug tomography (Pentacam, Oculus). OCT findings were correlated with clinical grading of ectasia.
The interval between PK and examination was significantly longer in eyes with ectasia compared with non-ectatic eyes in the study. There was a highly significant difference in lowest corneal thickness at the interface, graft-host interface angle and anterior chamber depth (in pseudophakic eyes) between the groups. The ratio calculated by the quotient of lowest corneal thickness at the interface divided by central corneal thickness (CCT) was significantly lower in ectatic than non-ectatic eyes. In eyes with a ratio of ≤0.7, the odds ratio for the occurrence of a clinical detectable ectasia was 2.4. Steep keratometry values were significantly higher in ectatic eyes.
The researchers thought it was interesting that there was a significant difference of several morphometric and keratometric parameters between the healthy control eyes and the post-PK eyes classified clinically as non-ectatic. “This could be explained either by the steep and thinned corneal recipient rim in keratoconus eyes or by early manifestation of ectasia, which is clinically not yet visible,” they wrote in their paper.
“The value of the morphological characterization of ectatic corneas using AS-OCT is limited insofar as the decision whether to perform surgical or other intervention is based on reduced visual function rather than altered corneal morphology,” the team pointed out. “Since objective and subjective measurements of refraction might prove to be difficult in ectatic eyes, AS-OCT measurements could serve as surrogate markers for progressive ectasia over time but should not be used for surgical decision-making.”
Weller JM, Hübner L, Kruse FE, Tourtas T. Characterization of ectasia after penetrating keratoplasty in keratoconus eyes using anterior segment optical coherence tomography. Br J Ophthalmol. March 20, 2023. [Epub ahead of print]. |

