 |
Q:
I have my first Boston KPro prosthesis patient (following severe stem cell deficiency) coming in next month for her first follow-up. There doesn’t seem to be much published on proper follow-up care of these patients. Any suggestions on what works best to minimize infection? Also, how to best estimate IOP, since conventional measures are not possible?
The Boston Keratoprosthesis (KPro) is a polymethylmethacrylate (PMMA) two- or three-piece prosthesis constructed similarly to a rivet through a traditional cornea (called the carrier cornea), explains cornea specialist Brandon Ayres, MD, of Philadelphia’s Wills Eye Hospital. The PMMA front plate of the prosthesis has a stalk that looks like a mushroom. The stalk is placed through a 3mm hole punched in the center of a traditional donor cornea, leaving the cap on the epithelial side. A titanium back plate is then snapped in place on the endothelial side of the carrier cornea, locking the prosthesis in place. Several small holes are drilled in the posterior plate to allow aqueous access to the cornea, which prevents melting of the carrier cornea (Figure 1).
“After surgery, most KPro patients wear a bandage contact lens to help prevent discomfort from the prosthesis and to help with tear distribution,” Dr. Ayres elaborates. “The KPro is a wonderful option for patients with multi-graft failure and other conditions where a traditional corneal transplant has a very low chance of success,” he explains. For example, cases of chemical injury and stem cell deficiency are prime candidates. The challenge of the KPro, however, is preventing infection and glaucoma progression.
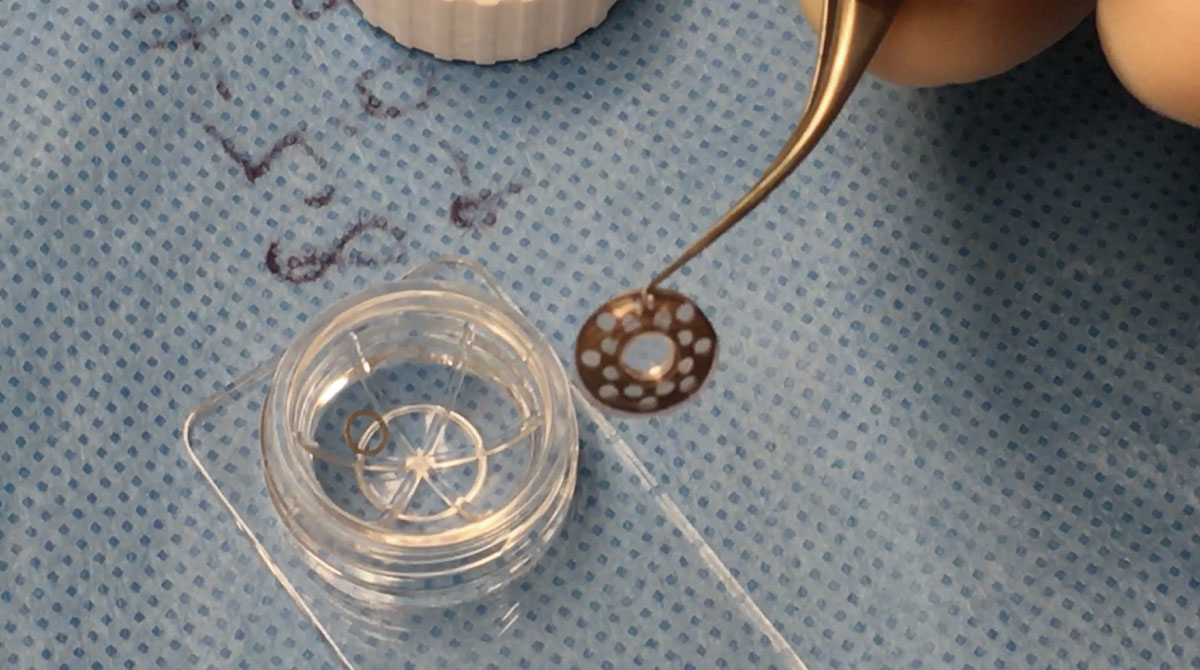 |
| Fig. 1. An intraoperative image of the Boston Keratoprosthesis. The PMMA front plate is held in place by a titanium back ring that “sandwiches” a human donor carrier cornea in place. The prosthesis will be sutured in place from carrier cornea to recipient cornea using 10-0 nylon suture. |
Management
In the case presented, the KPro is being placed due to limbal stem cell deficiency (LSCD). KPro is a good option for LSCD patients, preventing the need for autologous or cadaveric stem cell transplants. In cases such as this one, the surgery is the easy part; the challenge is following the patient for glaucomatous changes and infection prevention.
Many times, patients with stem cell deficiency also have a history of glaucoma. If a patient is already on glaucoma medications, a tube shunt may have already been placed or can be placed at the time of KPro surgery, which can make it much easier to regulate intraocular pressure, Dr. Ayres elucidates. In the event a tube was not placed, topical drops are still effective.
“The PMMA front plate makes it very difficult to accurately check the IOP of an eye with a prosthetic cornea,” explains Dr. Ayres. “As such, finger tension pressure should be checked on all patients every three to four months. Luckily, the KPro is clear from post-op day one, so the optic nerve can be directly visualized.”
Estimation of the cup-to-disc ratio should be documented every visit; a visual field and OCT should be performed every six months, Dr. Ayres counsels. It is also common to manage these patients in conjunction with a glaucoma specialist.
 |
|
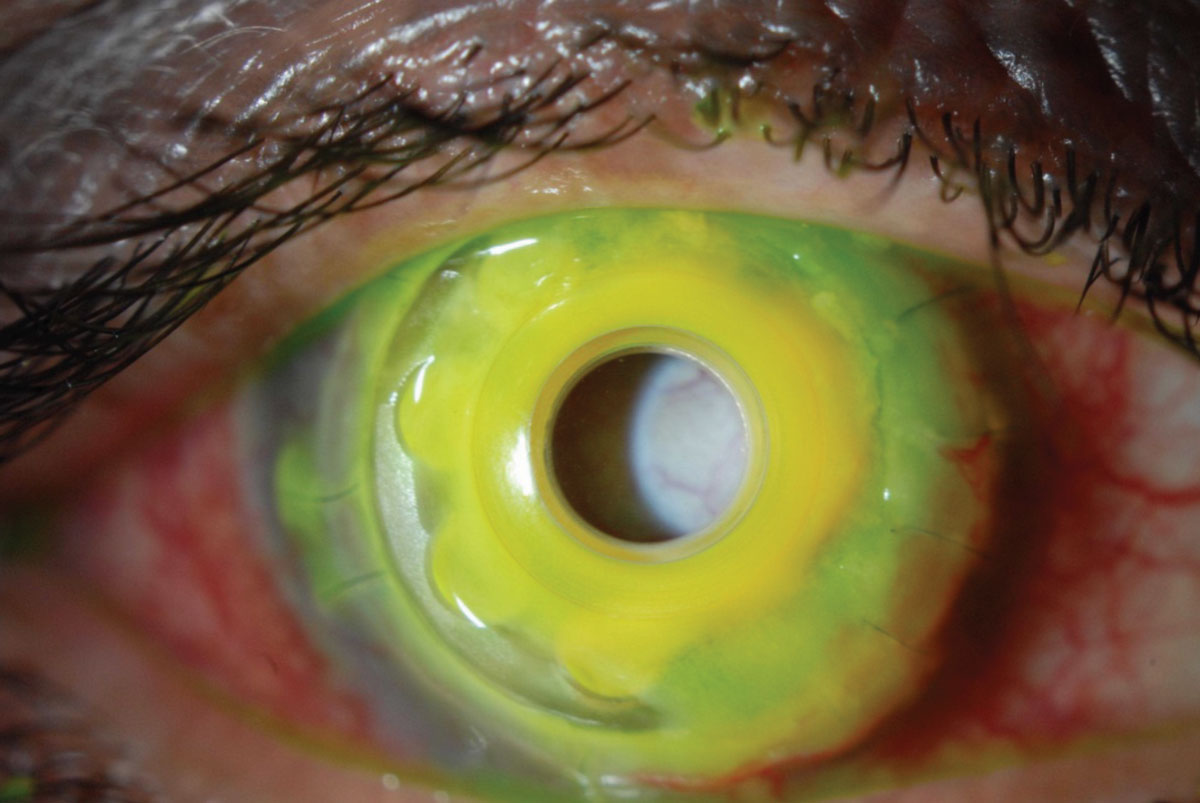
Fig. 2. A KPro with melting carrier cornea and fungal infiltrate around the stalk of the prosthesis. Note, this is an older version of the KPro with a PMMA back plate. Click image to enlarge. |
Preventing infection is critical in the KPro patient, and there are several acceptable medical regimens. Many patients are started on topical fluoroquinolone therapy four to six times daily after surgery and then tapered to once daily within the first two weeks post-op. The fluoroquinolone eye drop should be continued daily for life; very often, a drop of vancomycin (with concentration between 14mg/ml and 25mg/ml) is also used daily for life. An accepted alternative to this combination is to use polymyxin B/trimethoprim instead.
“In patients with severe stem ocular surface disease, as is often the case with LSCD, fungal overgrowth and infection (Figure 2) in the carrier cornea is a problem,” warns Dr. Ayres. To prevent this, amphotericin B (compounded) or natamycin (commercially available) can be pulsed twice daily during the first week of every third month. “In my own patients with LSCD, pulsing the antifungal has made a tremendous difference in the rate of fungal keratitis,” adds Dr. Ayres.
Lastly, the bandage lens needs to be managed in the KPro patient; almost any lens works. “We have patients who use daily, extended wear, hybrid and scleral contact lenses,” says Dr. Ayres. The lens will need to be changed according to its replacement schedule and how it looks during follow-up exams. “It is common to see deposits on the contact lens, indicating the need for change, but the lens is vital in preventing melting of the carrier cornea,” Dr. Ayres urges. “Best of luck with your patient—the KPro patient can be quite challenging!”
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.

