 |
A 55-year-old Black female presented with a chief complaint of blurry vision at near. Her systemic history was positive for hypertension, for which she was properly medicated and compliant. She denied allergies of any kind.
Diagnostic Data
Her best uncorrected entering visual acuities were 20/20 OD and 20/20 OS at distance, and 20/30 at near through her over-the-counter +1.50D reading glasses. Her external examination was normal, and there was no evidence of afferent pupillary defect. Biomicroscopic examination of the anterior segments was normal and Goldmann intraocular pressures were measured at 17mm Hg OU. The pertinent posterior segment findings are demonstrated in the photographs.
Additional studies included fundus photodocumentation, B-scan ultrasonography and optical coherence tomography (OCT) with a retinology referral and considerations for neuroimaging. Photos and OCT scans are shown below.
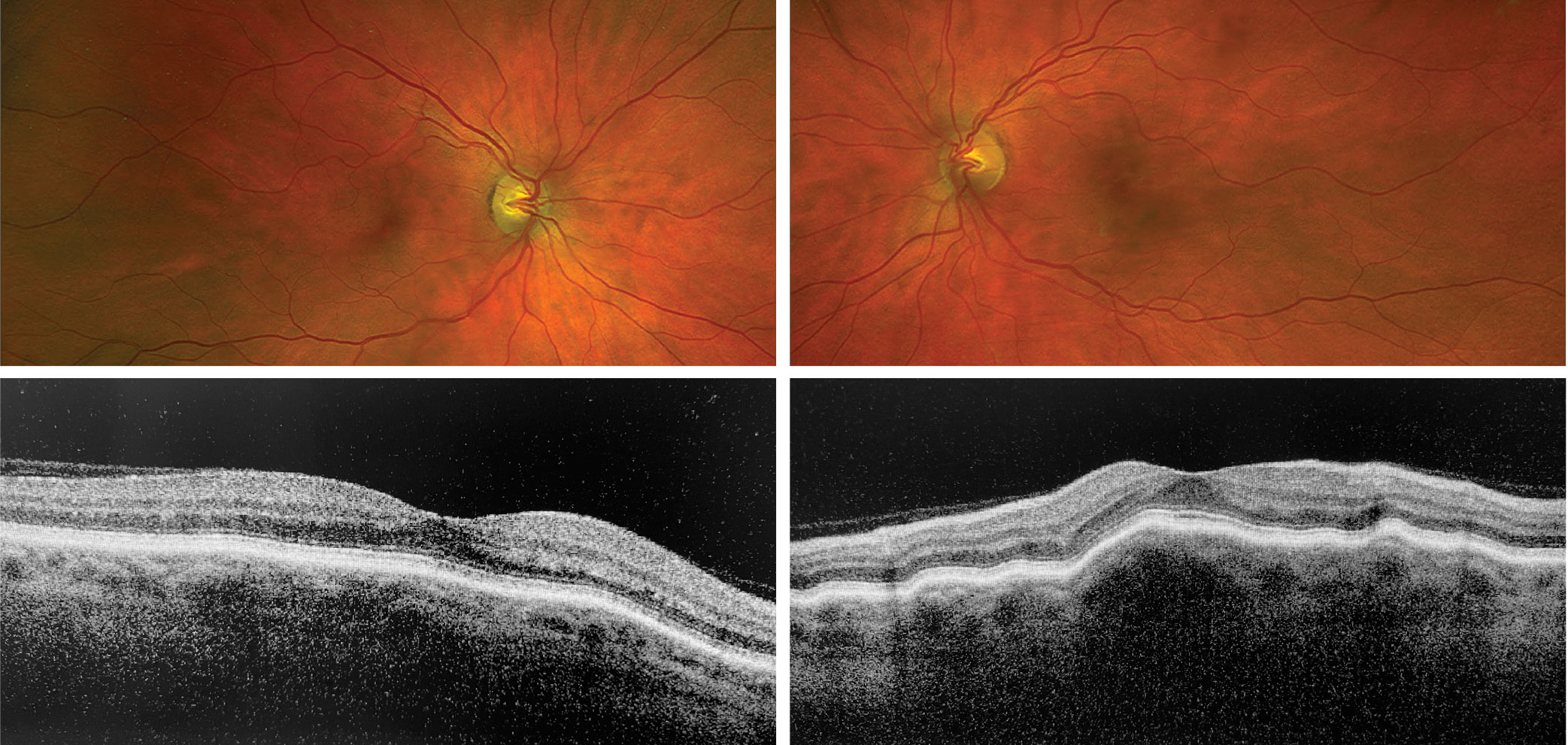 |
| What do these findings suggest about the patient? How would you approach management? Click to enlarge. |
Diagnosis
The diagnosis in this issue is idiopathic choroidal folds. This clinical entity creates the appearance of patterned striae in the fundus.1-12 They most often form idiopathically but are also associated with a variety of conditions.1-12 Folds can be described ophthalmoscopically as alternating light and dark streaks oriented horizontally, vertically, obliquely or at an irregular pattern within the posterior pole.1-8 Fluorescein angiography has been used to distinguish retinal folds (periodic surface undulations) from choroidal folds; however, the use of this technique is rare.6
Choroidal folds are also associated with a wide variety of pathological conditions, such as central serous chorioretinopathy, diabetes, choroidal nevi, posterior staphyloma, choroidal neovascularization, intra- and extraocular tumors, infiltrative ocular diseases, multiple myeloma, inflammatory diseases of the orbit, retinal detachment, scleral buckling and papillaedema.1-11 They may also occur as a secondary sequelae of intraocular surgical procedures or pharmaceutical treatments that produce temporary or chronic hypotony, such as cataract surgery, glaucoma surgery or medical glaucoma management.3,12 The literature also recognizes hypermetropia, optic disc drusen and the microgravity of space flight as benign conditions which may produce them.3,6
Histopathological observations made on enucleated eyes with choroidal folds found the common cause to be choroidal thickening due to vascular engorgement, hemorrhage or inflammation.13 Folds were also formed through tissue compression at the edge of choroidal tumors or via forces transmitted by scleral implants or by scleral thickening.13 Traction on the optic nerve and hypotony after paracentesis also created sufficient pulling to distort the underlying vascular layer and induce tissue “folding.”13 Retinal and choroidal folds are therefore possible via any mechanism which forces Bruch’s membrane to buckle.13
Clinical Implications
Choroidal folds are not a diagnosis, but rather a sign of underlying chorioretinal compromise. Idiopathic choroidal folds can only be determined by exclusion. There is generally no treatment, and they resolve spontaneously after the underlying cause is remedied. Idiopathic choroidal folds typically present no functional challenge. They only need to be monitored for changes that indicate something new is present or something old is changing.
Dr. Gurwood thanks Michael Rebar, OD, for contributing this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Goel N, Kumar V, Raina UK, Ghosh B. An unusual pattern of idiopathic choroidal folds. Oman J Ophthalmol. 2012;5(2):126-7. 2. Cohen SM, Gass JD. Bilateral radial chorioretinal folds. Int Ophthalmol. 1994-1995;18(4):243-5. 3. Jaworski A, Wolffsohn JS, Napper GA. Aetiology and management of choroidal folds. Clin Exp Optom. 1999;82(5):169-76. 4. Fagúndez Vargas MA, Jiménez Parras R, Bermúdez Uría L. Choroidal folds in diabetic retinopathy. Arch Soc Esp Oftalmol. 2000;75(12):797-802. 5. Kupersmith MJ, Sibony PA, Feldon SE, et al. The effect of treatment of idiopathic intracranial hypertension on prevalence of retinal and choroidal folds. Am J Ophthalmol. 2017;176:77-86. 6. Sibony PA, Kupersmith MJ, Feldon SE, et al. Retinal and choroidal folds in papilledema. Invest Ophthalmol Vis Sci. 2015;56(10):5670-80. 7. Jacobsen AG, Toft PB, Prause JU, et al. Long term follow-up of persistent choroidal folds and hyperopic shift after complete removal of a retrobulbar mass. BMC Res Notes. 2015;8:678. 8. Poon JS, Vahdani K, Booth AP. Chorioretinal folds in a patient with multiple myeloma treated with stem cell transplant. Eur J Ophthalmol. 2017;27(2):e46-9. 9. Kinoshita T, Imaizumi H, Miyamoto H, et al. Detection of choroidal folds in patients with Vogt-Koyanagi-Harada disease by retromode scanning laser ophthalmoscopy. Retin Cases Brief Rep. 2016;10(2):160-4. 10. Zwart SR, Gibson CR, Gregory JF, et al. Astronaut ophthalmic syndrome. FASEB J. 2017;31(9):3746-56. 11. Ishida T, Shinohara K, Tanaka Y, et al. Chorioretinal folds in eyes with myopic staphyloma. Am J Ophthalmol. 2015;160(3):608-13. 12. Parchand S, Kaliaperumal S, Deb AK, et al. Bimatoprost induced serous macular detachment after cataract surgery. Case Rep Ophthalmol Med. 2016;2016:7260603. 13. Bullock JD, Egbert PR. The origin of choroidal folds a clinical, histopathological, and experimental study. Doc Ophthalmol. 1974;37(2):261-93. |

