10th Annual Cornea ReportFrom advice on diagnosing and treating infections to managing trauma and limiting recurrent erosion, the April 2023 issue is full of clinical pearls to help you up your corneal management skills. Check out the other articles featured in this issue:
|
A relatively common condition, recurrent corneal erosion (RCE) is classically defined as a repeated detachment of the corneal epithelium in the presence of previous mechanical corneal trauma, dystrophy or degeneration.1,2 Some of the most common causes of mechanical injury involve fingernails, pet scratches, paper cuts and tree branches. Following trauma, the rate of RCEs can range from 5% to 25%.3
The condition can be extremely painful and disruptive to a patient’s life. Our job as clinicians is to treat them acutely and limit the number of recurrences.
Fortunately, today, there are many ways to treat an RCE depending on the severity of epithelial involvement and frequency of recurrence. Whichever method of treatment is chosen, the goal should always be patient comfort and reducing the likelihood of recurrent erosion. First-line therapies include topical and noninvasive options; however, surgery may be indicated for chronic episodes.
In this article, I’ll walk you through the pathophysiology, signs and symptoms, diagnosis and various treatment options for RCEs to equip you with the knowledge needed to best care for your patients dealing with this bothersome condition.
 |
|
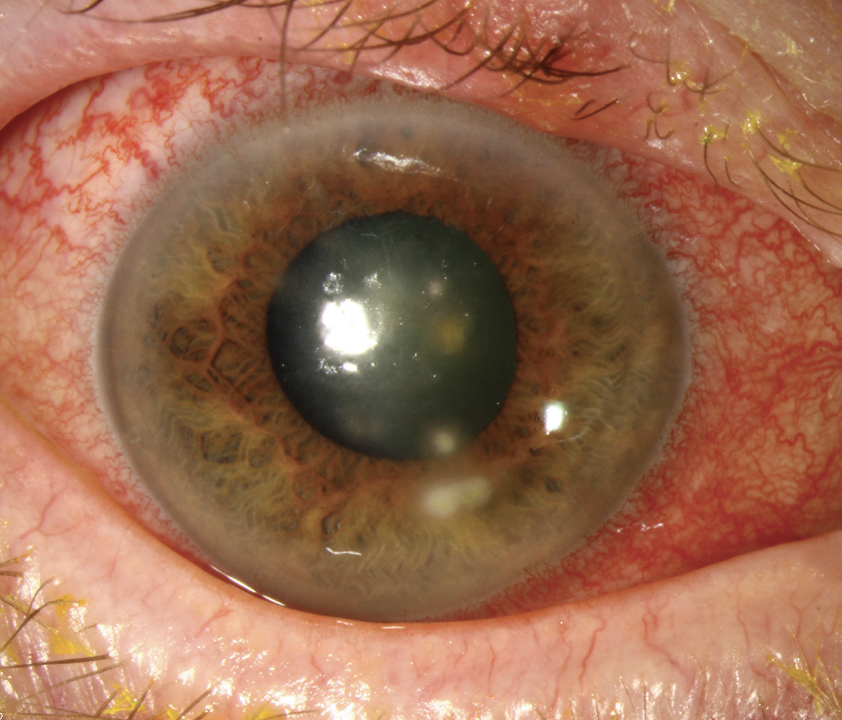
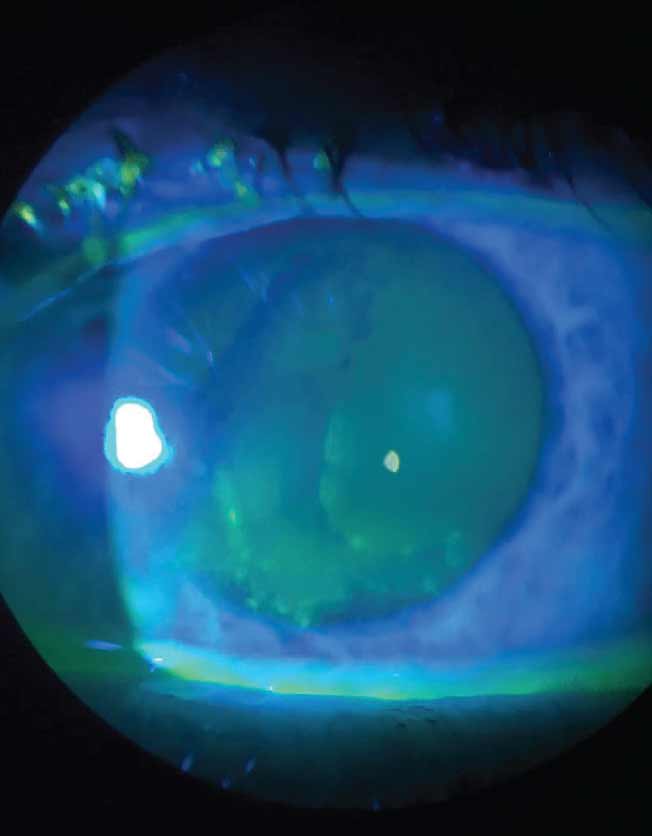
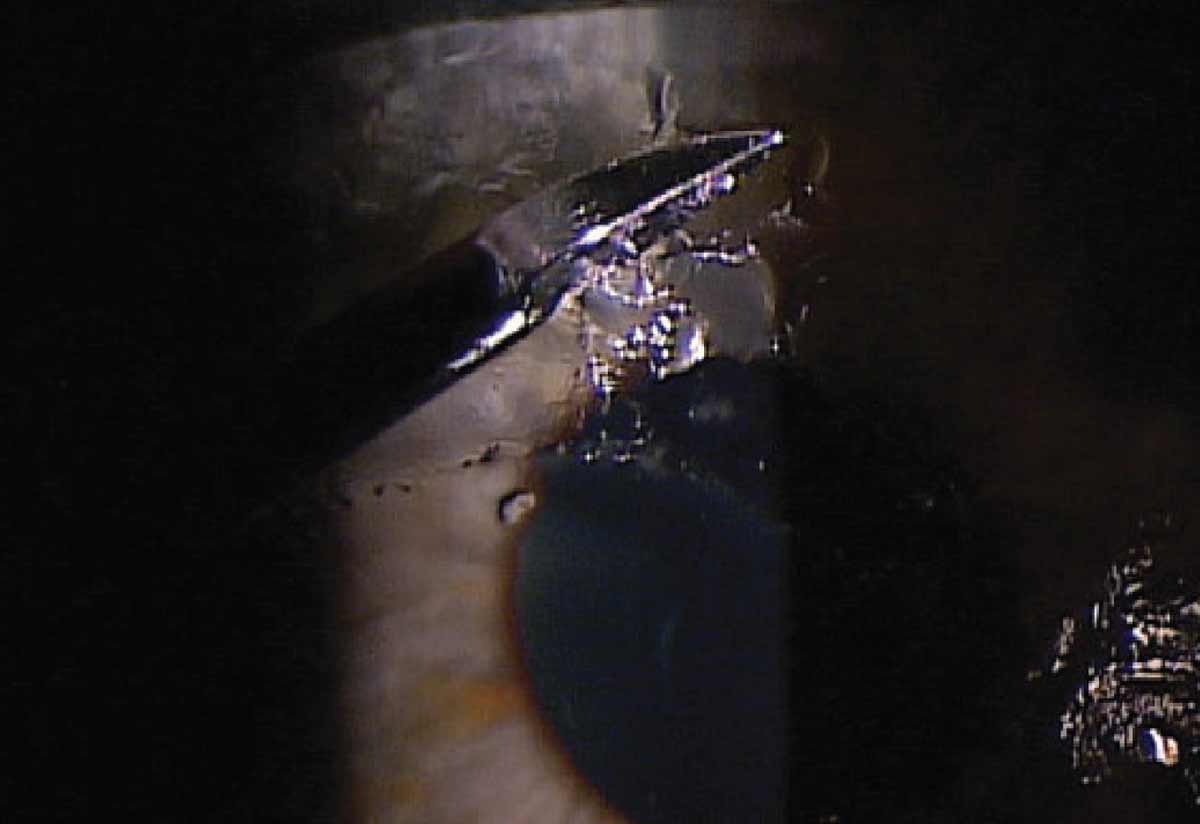
Fig. 1. Slit lamp view of fluorescein staining in a patient with anterior basement membrane dystrophy. Photo: Chris Kruthoff, OD. Click image to enlarge. |
Pathophysiology
Mechanical injury to the cornea leads to changes in the cell-to-cell and cell-to-matrix adhesions of the epithelial basement membrane. Changes specifically at the hemidesmosomes are the most likely cause of RCEs. Hemidesmosomes act as anchoring filaments to the basal layer of the corneal epithelium. After an injury, the hemidesmosomes disassemble to allow the cornea to heal. In RCE patients, these structures are frequently found to be compromised or missing altogether. This healing process can be slower in patients with diabetes, putting these individuals at increased risk of RCE development.4,5
Epithelial basement membrane dystrophy (EBMD) is most commonly characterized by visible map-dot or fingerprint-like patterns shown on slit-lamp examination. These patterns are caused by an abnormal basement membrane protruding into the epithelium. Presence of intra-epithelial pseudo-cysts and accumulation of intraepithelial material can also be found in varying degrees of EBMD. These redundancies and accumulation of irregular epithelial deposits lead to poor adhesion to the underlying structures when desquamating cells become trapped between the basement membrane and underlying structures. Up to 10% of patients with EBMD will experience RCEs.6
Signs and Symptoms
Patients with RCEs typically present in moderate to severe pain, which helps explain why this condition is a leading cause of eye-related emergency department visits. These episodes can be extremely debilitating and disrupt patients’ daily living activities. Affected patients will likely present with one or more of the following symptoms: sudden pain upon awakening, redness, photophobia, blurred vision and increased tearing.4,7 Any of these can last from hours to days depending on the severity of the erosion.
Upon examination, decreased best-corrected visual acuity may or not be present. A detailed slit-lamp examination will show variable degrees of disruption to the corneal epithelium. This can range from a small area of epithelial heaping to large areas of the epithelium being displaced or even missing. During the slit-lamp exam, an underlying corneal dystrophy or degeneration such as EBMD may be found and determined as an underlying cause of the RCE onset.
Fluorescein stain is essential in identifying and assessing the amount of epithelium involvement (Figure 1). Looking for areas of subtle epithelial movement when prodding with a cellulose sponge can reveal other areas of involvement as well. Conjunctival injection is also likely to be present.4,6,8
The recovery of the cornea from trauma involves a process of breaking down then repairing or rebuilding the damaged tissues. This process begins with inflammation with the increase in cytokines and an increase in matrix metalloproteinases (MMPs). While these factors are important in the inflammatory process, MMPs also play a role in the breakdown of the scaffold structured extracellular matrix. This matrix helps facilitate the rebuilding of the damaged tissues. Increased levels of MMPs can lead to the breakdown of this matrix too soon and inhibit proper repair of the epithelium and its underlying structures. Poor structuring in the repair process makes the epithelial cells prone to disconnect and could result in RCEs.1,2
The detachment of the corneal epithelium from the basement membrane during an RCE can have many causes, but the most common is the tear film drying out overnight. Combined with rapid eye movement cycles during sleep, this dryness can cause mechanical trauma to the cornea that results in an RCE and leads to an abnormally tight adherence of the eyelid to the corneal epithelium. The weak point of the junction with RCEs is typically the level of Bowman’s layer. Adhesion to the eyelid can be problematic during the rapid-eye-movement stage of sleeping and when opening the eye upon awakening. This is the typical cause of the classic “pain upon awakening” symptom that patients most commonly present with.4.8
Diagnosis
Initial presentation of an RCE can be difficult to diagnose without a thorough case history. They occur spontaneously, so it can be difficult for patients to link an event to the cause outside of instant pain upon awakening. Probing case history is most likely to uncover a previous ocular trauma. The second most common underlying condition is EBMD. Less likely but notable underlying conditions to inquire about or search for during examination include other corneal dystrophies and degenerations, refractive surgery, meibomian gland dysfunction and previous ocular surgeries.8
RCEs can be difficult to manage and often tend to recur despite active treatment, causing patients repeated episodes of pain and discomfort. There are many treatments available today including both medical and surgical options. The ideal treatment for each patient should be based on the severity of symptoms and the number of recurrences.
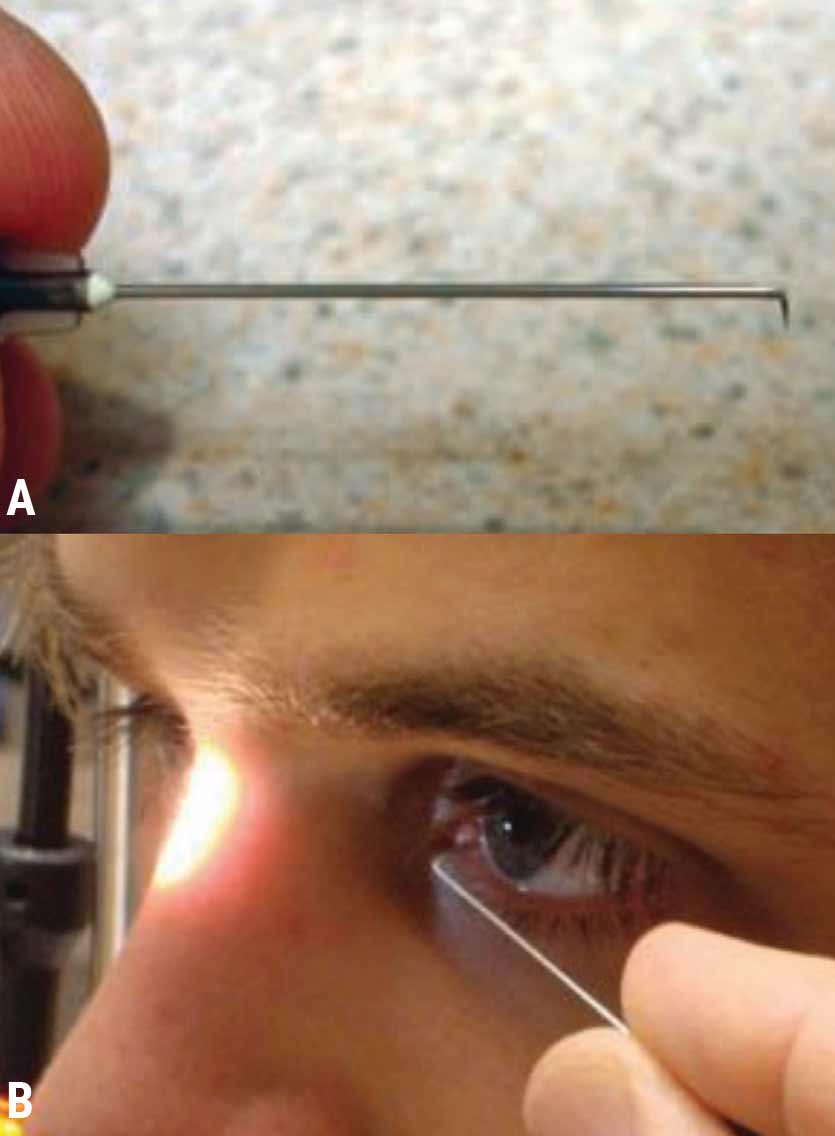 |
| Fig. 2. (A) Properly bent needle to perform anterior stromal puncture in the treatment of RCE. (B) ASP being performed tangential to the corneal plane. Photo: Nicholas Colatrella, OD. Click image to enlarge. |
Medical Treatments
Following an isolated incident of corneal trauma, a patient should be started on prophylactic treatment for three to six months to minimize the chances of an RCE.
Artificial tears are the first-line option for prevention and treatment of RCEs with few symptoms. Preservative-free artificial tears are recommended, but others can be used in their absence. The lubrication allows a buffer between the cornea and the eyelid that limits mechanical friction and adhesion of the cornea to the eyelid. This helps to promote healing for the cornea on its own accord without constant trauma from the lid. Failure with artificial tears and lubrication could indicate the need for punctal plugs to increase the tear lake and produce an equal or similar effect as drops.4,9
For RCEs with obvious epithelial defects, a topical antibiotic is indicated to help prevent infection from the compromised state of the cornea. Antibiotics such as topical fluoroquinolones and macrolide ointment are both appropriate forms of treatment. An oral nonsteroidal anti-inflammatory drug (NSAID) and/or topical cycloplegic can be added if the patient is in significant pain. Acetaminophen or ibuprofen are appropriate oral NSAIDs while 1% cyclopentolate is an appropriate cycloplegic dosing every 12 hours. Patients should never be allowed to self-administer topical corneal anesthetics for their pain.4,9
Painful RCEs may also indicate the installation of a soft bandage contact lens. This is to improve comfort for the patient by separating the damaged cornea from the constantly blinking eyelid. An extended-wear contact lens— silicone hydrogel being the most appropriate choice—should stay in the eye overnight and even for multiple days until the appropriate follow-up appointment. In severe cases, a cryopreserved amniotic membrane such as a Prokera can be another treatment option depending on need and availability. The main downside to Prokera lenses is that they are often not readily available and are usually expensive. Insurance coverage is not always guaranteed for Prokera, while a silicone hydrogel is likely available at most practices.4,9
Recurrent erosions with multiple recurrences can be treated more aggressively with autologous serum tears, MMP inhibitors and topical corticosteroids during the acute phase. Prophylactic antibiotic treatment is always recommended when using topical corticosteroids. These treatments help to decrease inflammation and promote proper healing of the cornea, which is essential to help limit recurrences.
Autologous serum tears can be an alternative lubrication option. Studies have shown that patients resistant to previous therapies have success with serum tears and fewer recurrences of RCEs. Allogeneic serum eye drops can even be an option for patients with poor venous access or severe anemia. These drops have a higher incidence of irritation and intolerance due to their allogeneic nature but remain an effective option when artificial tears are insufficient.4,8,9
MMP inhibitors such as oral tetracycline have been shown to be effective as a next-line therapy. MMPs promote the breakdown of hemidesmosomes and collagen so that MMP inhibitors can help promote strength in those connections and corneal structures.1,4,9
Corticosteroid drops such as loteprednol, fluorometholone or prednisolone acetate work to decrease inflammation and promote healing. They are best indicated after failed attempts at lubrication and punctal occlusion.1,4
Corticosteroid drops used in combination with MMP inhibitors can effectively inhibit MMPs as well as down-regulate the production of lipase. There is evidence to suggest that meibomian gland dysfunction is a risk factor for RCE, and this drug combination can help improve gland dysfunction symptoms.1,4
After resolution of an acute RCE, a hypertonic solution or ointment is often recommended for long-term therapy. Once the corneal epithelial defect is closed, these agents can help remove edema from the cornea through osmosis. The removal of this swelling allows the structures in the cornea to regrow closer to each other and promotes tighter adhesion. These hypertonic agents can be used for six to 12 months after the initial onset of RCE.4,5
Surgical Options
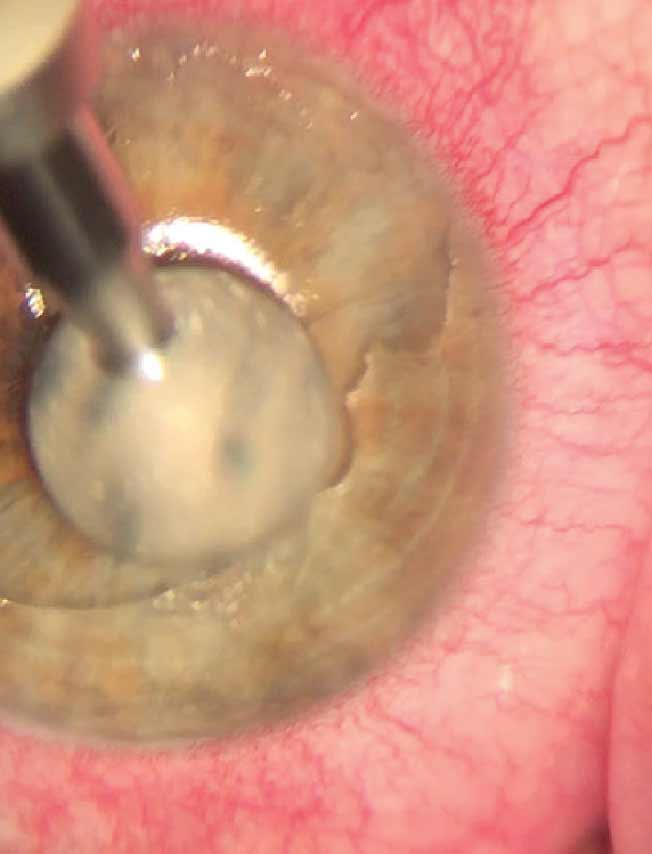 |
| Fig. 3. Slit lamp view of a debridement of the corneal epithelium under topical anesthesia using a foreign body spud. This procedure is effective for treating active acute RCE. Photo: Nathan Lighthizer, OD. Click image to enlarge. |
Medical management is often not sufficient to treat persistent RCE. In these more severe cases, surgical intervention may be necessary to help accelerate recovery of poorly healing lesions.
A common first-line surgery to manage stubborn RCE is anterior stromal puncture (ASP) (Figure 2). The most common practice of ASP involves anesthetization of the cornea followed by puncturing Bowman’s layer with a bent 25- or 27-gauge needle, roughly 0.5mm apart. This process helps to promote stronger adhesion of the epithelium to Bowman’s layer.4,9-11
A similar method of ASP uses a Nd:YAG laser instead of a needle to make the punctures in Bowman’s layer. The benefit of the Nd:YAG laser is that the puncture’s are shallower and more consistent, which, in theory, should lead to less corneal scarring.
It’s important to note that these two methods of ASP only work for peripheral RCE lesions due to the high risk of scarring. Scarring on the peripheral cornea should not affect best-corrected visual acuity; however, there is a risk for the patient to have increased glare. Developments in ASP using OCT to map the anterior segment can provide a more detailed image of the injured area and enable more precise treatment, allowing for fewer punctures and, in turn, less scarring.4,9-11
Note that ASP and Nd:YAG laser are not usually indicated for central RCEs but rather are typically reserved for off-axis injuries. There are other surgical options that are more effective for central corneal epithelial defects, including diamond burr superficial keratectomy and phototherapeutic keratectomy (PTK).
Epithelial debridement is an effective and common treatment for active RCEs (Figure 3). The damaged tissue is mechanically removed with a cellulose sponge or blunt spatula. This clears the area for proper regeneration of epithelial tissue. Afterwards, a bandage contact lens should be placed, and the patient should be prescribed corticosteroid drops and a topical antibiotic while they recover. This treatment is extremely effective at managing acute RCEs but not at limiting the chance of recurrence.4,9-11
 |
|
Fig. 4. Diamond burr superficial keratectomy is a variation of epithelial debridement that uses a diamond burr to remove the damaged tissue, creating a smooth surface at the level of Bowman’s layer. Note that while this method is highly effective at limiting recurrences, it does have a longer recovery time for the patient than other procedures. Patients may also experience corneal haze and increased pain during healing, which topical corticosteroids can help to alleviate. Photo: Aaron McNulty, OD. Click image to enlarge. |
Diamond burr superficial keratectomy is an alternative treatment that has been shown to be the most effective method of reducing RCE recurrence (Figure 4). It is a variation of epithelial debridement that uses a diamond burr to remove the damaged tissue without puncturing Bowman’s layer and thus can be used safely on central RCE lesions with limited risk of scarring. The diamond burr helps to create an extremely smooth surface on Bowman’s that allows for proper regrowth while also possibly stimulating extracellular matrix proteins. This stimulation promotes stronger adhesions and connections to Bowman’s layer and may help reduce recurrence rates.
While diamond burr superficial keratectomy is very effective at preventing recurrence, one of its downsides is the long recovery time for the patient. The process also can cause corneal haze during healing which may frustrate patients with blurry vision. The technique also often increases the amount of pain in recovery. Topical corticosteroids can be used in combination to limit corneal haze and accelerate patient recovery and discomfort.4,9-11
PTK has also shown effectiveness in treating RCEs and limiting their recurrence rates. This laser treatment ablates the superficial layers of the corneal past Bowman’s layer and slightly into the anterior stroma. Due to the effect of the laser, there is no trauma response from the cornea, decreasing the risk of scarring. This makes the treated surface exceptionally smooth and, in turn, helps promote proper healing. A smooth surface for the epithelial basement membrane to bond to promotes stronger adhesions, specifically at the level of the hemidesmosomes. As with diamond burr polishing, the smooth surface is key to improving long-term results for RCE patients.
The biggest downfall of PTK is the cost and requirement of a surgical suite. It can also cause changes to refractive error, specifically increased astigmatism due to the depth of the therapy.4,9-11
A more recent treatment option called alcohol delamination has shown great promise in reducing recurrence rates. This process involves applying small amounts of diluted alcohol to an anesthetized cornea. After the alcohol is removed with a sponge, the damaged epithelium peels off easily. This process minimizes haze due to the removal of only the superficial corneal epithelium, an advantage that alcohol delamination has over diamond burr superficial keratectomy. Postoperatively, patients should use preservative-free artificial tears, take a topical antibiotic and wear a bandage contact lens for around one week.4,9
The goal of all these surgical treatments is to remove the compromised corneal tissue and allow new tissue to grow with stronger adhesive complexes. A smooth surface allows for cellular matrix structures to form tighter junctions and adhesions, ultimately leading to fewer recurrences.
To see a flowchart that outlines the various therapeutic options for managing RCE with or without epithelial defect, refer to the protocol outlined below.
RCE Treatment Protocol Recommendations
First-time acute RCE with epithelial defect treatment options:
Recurrent acute RCE with epithelial defect options (can use any or all in addition to the first-time acute RCE treatment options above):
Potential surgical options in cases of repeated recurrent episodes:
After resolution of RCE (healed epithelium):
|
Patient Reassurance
To help manage expectations of pain and discomfort for patients with RCEs, it’s essential to educate them about the condition and various management options throughout follow-up. The anxiety of not knowing when an RCE will occur can be one of patients’ biggest concerns. When managing these patients, especially those with numerous recurrences, exhibiting empathy and taking time to discuss the range of treatment options can be reassuring and help to establish patient trust and confidence. For patients that have struggled with RCEs for years, knowing that there are other interventions to try if one fails can help them feel more optimistic about treatment.
Takeaways
Topical and surgical treatments give physicians many options when treating RCEs. Guiding your treatment towards the unique situation that presents is the best way to ensure positive long-term results. Escalating our aggressiveness with treatment options depends on factors such as severity and frequency of recurrence.
Becoming familiar with the numerous treatment options you have at your disposal can help reduce recurrent episodes and improve your patients’ quality of life. RCEs can be frustrating for patients and physicians alike, but limiting recurrence is key.
Dr. Saeli is a staff optometrist at the Cincinnati VA Medical Center and serves as adjunct faculty at Ohio State University. He has no financial disclosures.
1. Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-35. 2. Tsatsos M, Matsou A, Soultanidis M, Athanasiadis IK. Safety and efficacy of hypertonic sodium chloride 5% ointment for recurrent corneal erosion syndrome. Cureus. 2022;14(12):e32796. 3. Albert D, Miller J, Azar D. Recurrent corneal epithelial erosion. Albert & Jakobiec’s principles and practice of ophthalmology. Philadelphia: Saunders/Elsevier. 2008. 4. Lin SR, Aldave AJ, Chodosh J. Recurrent corneal erosion syndrome. Br J Ophthalmol. 2019;103(9):1204-8. 5. Dursun D, Kim MC, Solomon A, Pflugfelder SC. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix metalloproteinase-9, doxycycline and corticosteroids. Am J Ophthalmol. 2001;132(1):8-13. 6. Wong VW, Chi SC, Lam DS. Diamond burr polishing for recurrent corneal erosions: results from a prospective randomized controlled trial. Cornea. 2009;28(2):152-6. 7. Watson SL, Lee MH, Barker NH. Interventions for recurrent corneal erosions. Cochrane Database Syst Rev. 2012;(9):CD001861. Update in: Cochrane Database Syst Rev. 2018;7:CD001861. 8. Buffault J, Zéboulon P, Liang H, et al. Assessment of corneal epithelial thickness mapping in epithelial basement membrane dystrophy. PLoS One. 2020;15(11):e0239124. 9. Chen YT, Huang CW, Huang FC, Tseng SY, Tseng SH. The cleavage plane of corneal epithelial adhesion complex in traumatic recurrent corneal erosion. Mol Vis. 2006;12:196-204. 10. The Wills Eye Manual: office and emergency room diagnosis and treatment of eye disease. Philadelphia: Lippincott.1994. 11. American Academy of Ophthalmology. Corneal abrasion and erosion. Published September 26, 2022. www.aao.org/eye-health/diseases/what-is-corneal-abrasion. Accessed March 20, 2023. |