10th Annual Cornea ReportFrom advice on diagnosing and treating infections to managing trauma and limiting recurrent erosion, the April 2023 issue is full of clinical pearls to help you up your corneal management skills. Check out the other articles featured in this issue:
|
Simply put, the cornea protects our eye. So, when the cornea experiences trauma, such as corneal injuries, abrasions and foreign bodies, it must not be taken lightly.
Globally, corneal injuries comprise the majority of ophthalmic cases in the emergency room.1 The leading cause of blindness in children and young adults is ocular trauma that traditionally happens during recreational activities.2
Corneal abrasions are the number one form of ocular trauma and can arise from contact with a variety of materials, including dirt, wood, plants, metal, paper and fingernails.3
Corneal foreign bodies are another type of commonly seen corneal trauma, second only to abrasions. They are oftentimes superficial and consist of materials similar to what causes abrasions.
Additional forms of corneal trauma consist of injuries from chemical, thermal or radiation sources. Management varies depending on severity, but many conditions can be taken care of in-office. Here, we will discuss how to properly manage corneal trauma, along with etiologies of each to prepare you for when you see these types of cases come through your practice.
Corneal Injury Pathophysiology
This injury can be extremely painful due to the rich innervation of the corneal epithelium, which is four to six cell layers thick and can regenerate completely in about one week.4 When the epithelial integrity is compromised, new cells rapidly proliferate to cover the wound.4 The limbal stem cells regenerate corneal epithelium and remodel the basement membrane layer of the cornea.4 This allows the cornea to heal by proliferating new cells that migrate to and fill in the corneal defect.
Healing time depends on the size and depth of the injury. Initially, the limbal stem cells will make a layer of epithelial cells to cover the wound. This “covering” will reduce pain significantly for the patient. Full healing requires the corneal epithelium to return to normal by proliferating cells and remaking cell adhesions to restore the strength of the cornea. Those with wounds where the cellular adhesions do not return to normal or those with certain corneal dystrophies are at risk for recurrent corneal erosions because the epithelium is in a constant weakened state.4
The corneal stroma is made up of keratocytes that are organized by collagen fibrils and proteoglycans. When corneal trauma creates deeper wounds into the stroma, healing time will be lengthened. Stromal wound healing involves proliferation of keratocytes which then migrate and differentiate into myofibroblasts. Myofibroblasts will then produce an extracellular matrix and proteinases which contract and close the wound. The proteinases then create an immune response which clears debris and helps prevent infections. This also allows the basement membrane to regenerate. When this cascade works as described, transparency of the cornea is reestablished. When the cascade is interrupted, a corneal opacity will result.5
After any corneal trauma, a full ocular health evaluation is warranted and careful examination of the anterior segment is essential.6 Using ocular surface dye, such as sodium fluorescein, is helpful to identify the extent of injury. Sodium fluorescein can also assist in identifying a penetrating corneal injury by a positive Seidel test. With any corneal trauma, it is recommended that the provider dilates the patient. This is especially important in injuries that arise from high-speed trauma, hot metal to the eye and grinding trauma in order to rule out intraocular foreign body with a self-sealed or cauterized corneal wound.
Corneal Abrasions
Despite the multitude of causes and presentations that abrasions may comprise, principles of care are fairly consistent.
Etiologies. Abrasions are scratches or injuries to the surface epithelium of the cornea and represent the most common form of ocular trauma. They may be caused by a variety of factors, such as trauma to the eye, foreign bodies, contact lens wear or underlying ocular disease. Patient symptoms can include pain, redness, tearing, photophobia, blurred vision and foreign body sensation.
In most cases, corneal abrasions heal within one to seven days; however, if the abrasion is very large or deep, the healing time can be longer.1 Assisting in healing by use of medical treatment is necessary in almost all cases.
Recurrent corneal erosions are another type of corneal abrasion that occurs from a history of corneal trauma or corneal dystrophies where the epithelium was not able to restore the organization of cellular adhesions during the healing process. This puts the cornea at a higher risk of recurrent erosion and abrasions in the location of previous trauma. These commonly occur upon waking.
 |
|
Fig. 1. Corneal abrasions stained with fluorescein and visualized using a cobalt blue light. Photo: Leslie Cecil, OD. Click image to enlarge. |
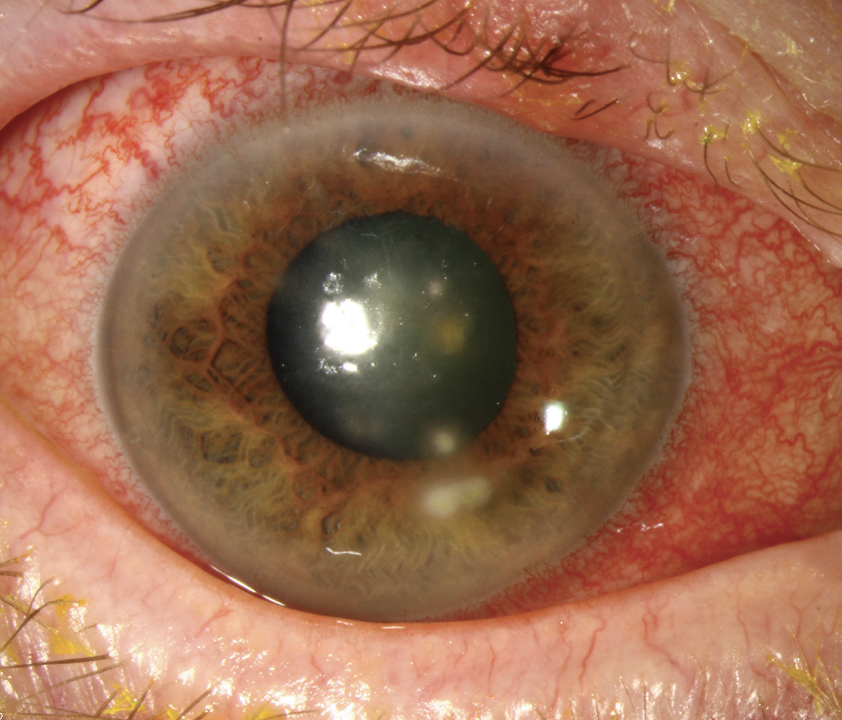
Management. Any corneal trauma should be evaluated with a slit lamp. Due to the pain that corneal epithelial damage causes, topical anesthetics can greatly increase ease of examination, but should never be dispensed to the patient. Firstly, after initial exam, instilling sodium fluorescein will help identify the extent of the corneal defect and make any corneal damage noticeable upon using the cobalt blue light, either from a slit lamp or handheld light source.
Abrasions have many different shapes and sizes, and it is important to photodocument or measure the size of the defect for management and follow-up purposes. Determining the cause of abrasion is necessary to establish a plan of treatment. Occasionally, the causative object is still present in the conjunctival sulcus. If the staining pattern is vertical, this may indicate a residual foreign body under the lid.7 Everting the lid and irrigating the eye is critical here.
If there is any nonadherent or loosely adhered epithelium, debridement may enhance the healing process.8 This procedure is done at the slit lamp using topical anesthesia. A foreign body spud or cellulose surgical sponge can be used to debride the loose tissue and provide a smooth basement membrane which allows for a better chance of epithelial re-adherence.8
Using topical antibiotics is the mainstay of treatment for corneal abrasions. For large abrasions greater than 4mm, topical cycloplegics, such as cyclopentolate, can also be used.9 Patching for larger abrasions was previously recommended; however, it’s no longer standard of care.10 The Corneal Abrasion Patching Study Group found that traumatic, noninfected abrasions not arising from contact lens wear could safely be treated with antibiotics and cycloplegics without the need for a pressure patch.10
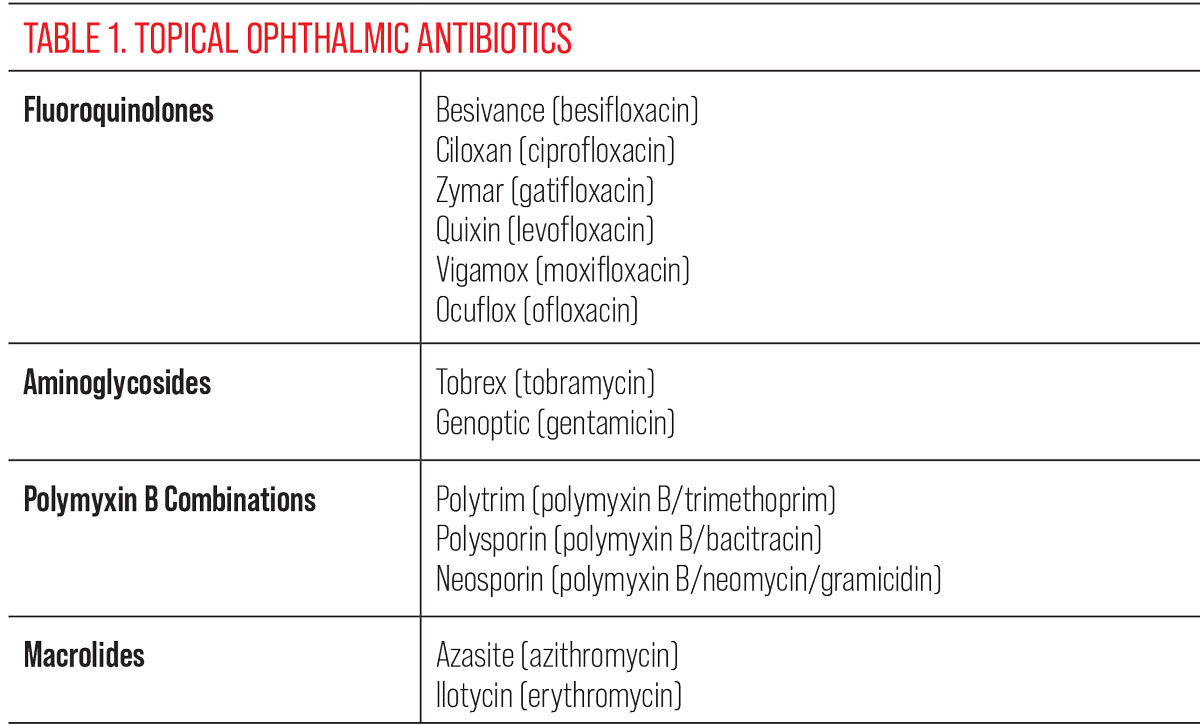
Topical treatment options include ophthalmic lubricants, cycloplegics and antibiotics, including fluoroquinolones, amnioglycosides, polymyxin B combinations and macrolides (Table 1). Many of these also come in ointment formulations that can be used to enhance comfort while healing and for overnight use. Many studies have been done regarding which antibiotic performs better, and the conclusions show that there is insufficient evidence to support whether one regimin outperforms another.11
If the corneal trauma is secondary to contact lens use, a fluoroquinolone or aminoglycoside is the drug of choice due to pseudomonas coverage. Antibiotic use is commonly dosed two to four times per day in the affected eye. Duration depends on size and depth of abrasion, and discontinuation is appropriate when the epithelium is healed.
For pain control, oral nonsteroidal anti-inflammatory drugs (NSAIDs) can be useful. Ophthalmic topical NSAIDs have not been shown to be beneficial in the same way oral NSAIDs can be.9
Cycloplegics can also be used for pain control due to discomfort from ciliary spasm. This is not as commonly used, but medication choices consist of cyclopentolate and homatropine.9 These are more commonly used if there is a concurrent iridocyclitis along with the initial traumatic abrasion.
FDA-approved bandage contact lenses are sometimes used when the abrasion is large in order to increase patient comfort.
If the abrasion is non-healing, consideration can be made for an amniotic membrane.
CASE REPORT
A 25-year-old male presented to Urgent Care with new-onset eye pain, redness and decreased vision in his left eye after a walk through the woods with his dog the day prior. The Urgent Care provider referred the patient to us and he was evaluated in our office.
Entering visual acuities were 20/20 OD and 20/40 OS. Intraocular pressure (IOP) was 14mm Hg OD and 12mm Hg OS. Pupils were equal, round and reactive with no afferent pupillary defect detected. Extraocular motility was also normal in both eyes. Slit lamp examination revealed a 3mm by 2mm corneal abrasion with positive sodium fluorescein staining of the lesion on the left cornea. Anterior chamber was free from cells and flare. Dilated fundus examination of both eyes was unremarkable.
A corneal abrasion of the left eye was diagnosed. The patient was educated on healing time and given ofloxacin 0.3% to use TID OS for one week. A follow-up was scheduled for one week later.
At follow-up, the left eye corneal epithelium was completely healed without any sodium fluorescein uptake and vision returned to 20/20 OS. The ofloxacin was discontinued.
 |
Corneal Foreign Bodies
Optometrists are increasingly called upon to not simply triage corneal foreign bodies but also remove them, as scope laws and optometric training are evolving to better meet the needs of the public.
Etiologies. Commonly occurring in the workplace, corneal foreign bodies are the second most common form of ocular trauma. The best protection against corneal foreign bodies is protective eyewear. Failure to consistently wear eye protection increases the risk of serious ocular harm. Foreign bodies are typically superficial and can cause significant ocular discomfort. Rarely, they can embed and even penetrate the cornea.12
Management. The origin of the foreign body must be determined and removal should happen as quickly as possible using one of many different techniques. Irrigation can remove superficial foreign bodies quite well and is less invasive than other methods. However, if the foreign body is deeply embedded, a 25- to 30-gauge beveled needle or a stainless steel spud can be used under slit lamp to assist in removal. An Alger Brush with burr or a Bovie burr can be used to eradicate a foreign body as well, but it is most frequently used to remove a rust ring leftover from metallic foreign bodies.15
Metallic foreign bodies can be removed with a low risk of infection; however, they have a higher risk of scarring after the procedure. Rust can remain after removal of the initial foreign body. It is sometimes appropriate to re-evaluate the patient a few days after the initial removal to eliminate remaining rust that has moved anteriorly. If the abrasion is large or central post-foreign body removal, it is common to issue topical prophylactic antibiotic coverage.
If a foreign body is organic in nature, the risk of infection is higher, and the patient should be monitored closely for development of bacterial or fungal keratitis post-removal. It would also be appropriate to issue a topical broad-spectrum prophylactic antibiotic in this case.
If a foreign body is posterior to the posterior stroma or Descemet’s membrane, it is recommended that the foreign body be surgically removed by an ophthalmologist emergently.12 Rarely, there can be penetrating foreign bodies without an obvious outlet. In these cases, imaging, such as OCT, B-scan and CT, can be beneficial.
CASE REPORT
A 59-year-old male presented with a foreign body sensation and blur OS. He reported that he felt something in his eye a week ago and the blur hadn’t subsided. No eye drops had been used.
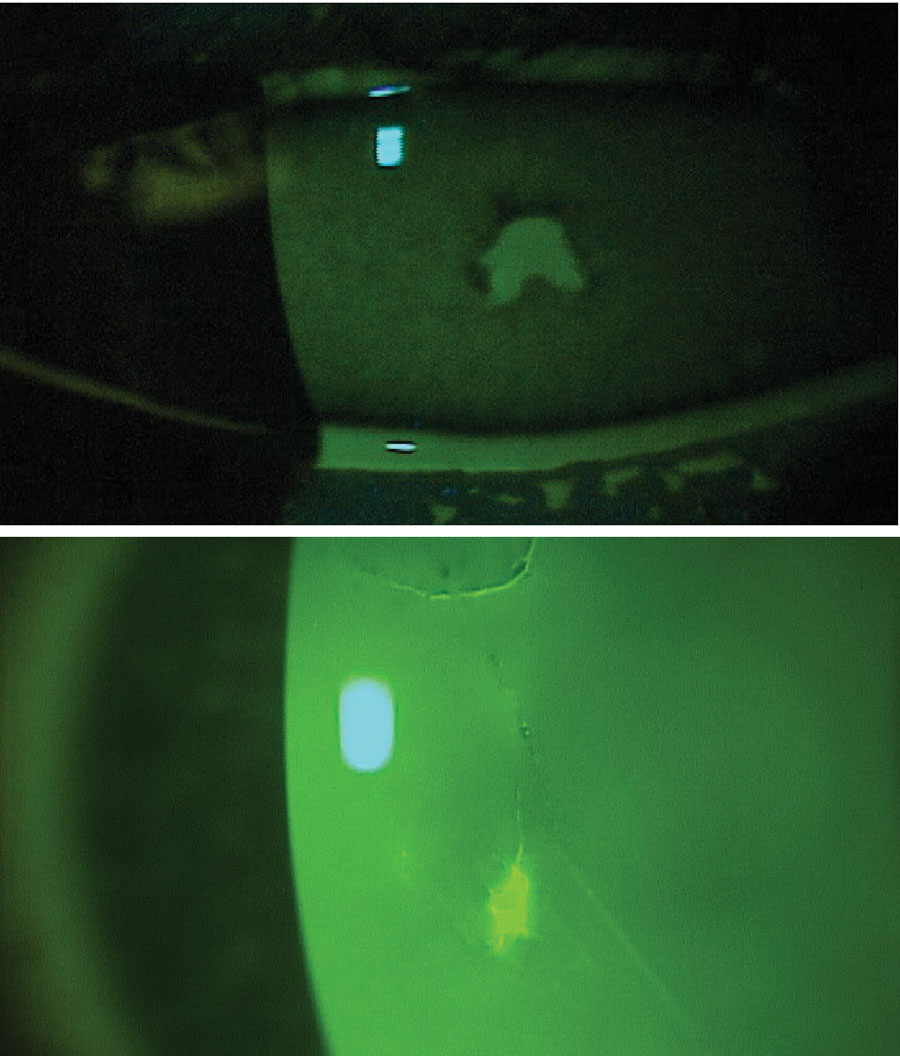
Entering visual acuities were 20/20 OD and 20/200 OS. IOP was 10mm Hg OD and 16mm Hg OS. Pupils were equal, round and reactive with no afferent pupillary defect detected. Extraocular motility was also normal in both eyes. Slit lamp examination revealed a small metallic foreign body with rust beginning just inferior to the central visual axis (Figure 2A). The anterior chamber was free from cells and flare. Dilated fundus examination of both eyes was unremarkable.
Removal occurred using a stainless steel foreign body spud which removed the superficial metallic piece. A small, imbedded metallic foreign body remained, and a Bovie spud was needed to remove it completely (Figure 2B). After the entire foreign body was removed, a small superficial wound remained (Figure 2C).
The patient was given ofloxacin twice per day OS and scheduled for a follow-up two weeks later. Upon return, the corneal epithelium was healed completely with a small scar beginning to form.
 |
|
Fig. 2. (A) Metallic foreign body with early rust proliferation embedded in the central cornea. (B) Remaining metallic foreign body after the superficial metal was removed with a foreign body spud. (C) Corneal abrasion with sodium fluorescein uptake remaining after removal of a metallic foreign body. Click image to enlarge. |
Exposure-related Corneal Trauma
Corneal exposure to a chemical is an emergency and requires prompt evaluation and management.
Etiologies. The vast majority of these injuries are accidental.13 There are two types of chemical burns: acid burns and alkali (basic) burns. Acids that are frequently contacted are from swimming pool cleaners and car batteries, and are generally milder than their base counterparts.14 Acids with a pH less than four can impact the corneal epithelium and cause damage by denaturing the corneal epithelial cells.14 Most acids will produce corneal proteins upon contact, which slows penetration and reduces destruction. Alkali chemicals are lipophilic, which allows them to penetrate cell membranes via membrane lipids permitting further chemical penetration of the cornea.14 Common bases that are regularly available are found in cleaning products, such as lye or ammonia, and calcium hydroxide in cement or plaster.
There are numerous classification schemes available to grade ocular chemical injuries. The basis of these grading systems is to determine corneal, conjunctival and limbal damage at the initial assessment.13 Though specific rationales differ, they are largely based on the degree of perilimbal ischemia and corneal haze. The prognosis is worse with a greater initial level of ischemia and haze.
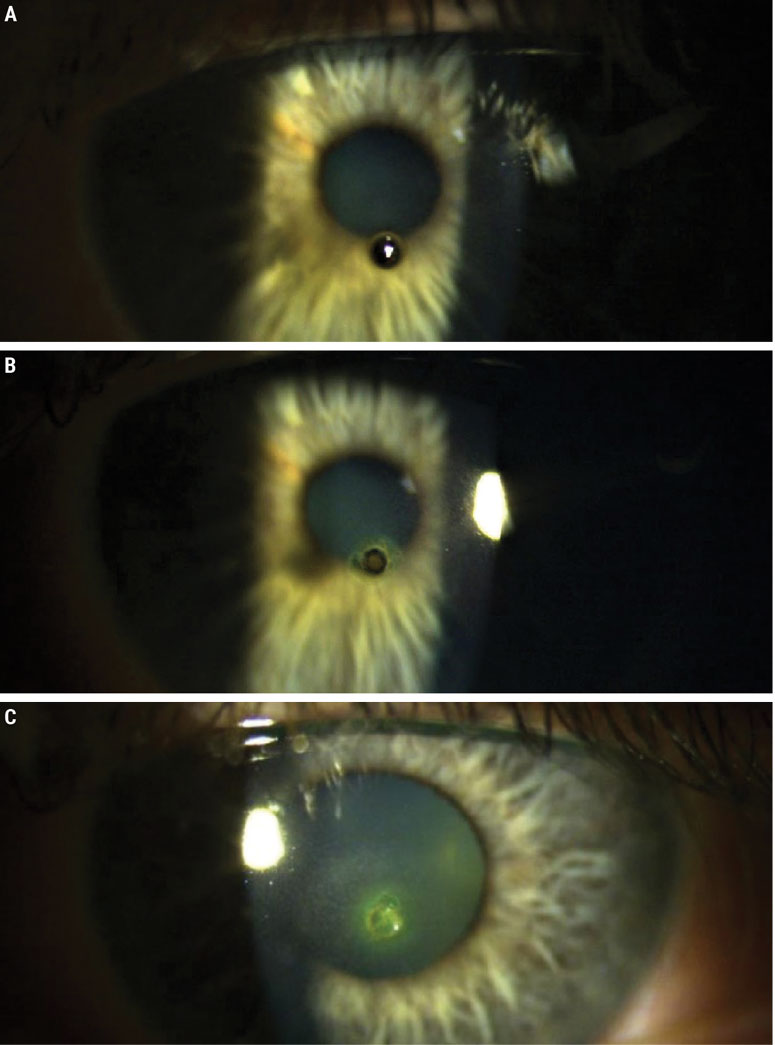
Management. When a chemical corneal exposure case presents, time to dilution of the chemical is directly related to visual outcome. The most important step is copious irrigation to dilute and remove the offending agent. This irrigation can happen at the site of the incident or in office prior to a complete exam. After irrigation for five to 10 minutes, pH can be tested using litmus test strips, and when the goal of 7.0 to 7.4 pH is met, dilution is complete.14
Tap water has been shown to be an appropriate solution for irrigation due to its widespread availability in most settings. Balanced salt solution or saline solution are better options for irrigation in a clinical setting and also preferred options in an emergency settings if obtainable. Balanced salt solution has been shown to neutralize the pH faster than water.14
In mild chemical injuries, antibiotics such as erythromycin and bacitracin, usually in an ointment formulation, are typically used.14 Use of a steroid, such as prednisolone acetate dosed four times per day, can be helpful to reduce inflammation during the healing process. Preservative-free artificial tears are also helpful for comfort while keeping the eye lubricated. If there is more discomfort and pain, a cycloplegic can be used.
Follow-up care should occur frequently until the entire cornea has healed.
More severe chemical injuries require an aggressive medication regimen for management. Cycloplegics for pain control, prednisolone acetate hourly while awake, antibiotic solutions four times daily and oral NSAIDs to help control pain are all parts of severe chemical injury treatment.
The use of an amniotic membrane graft is also found to be beneficial in certain cases; however, when to initiate this treatment is controversial. Nevertheless, follow-up should be daily until re-epithelialization is adequate. Careful monitoring of IOP is important; if it is elevated, alpha agonists should be avoided due to their vasoconstrictive properties.14 Follow-up every other day to one week thereafter is acceptable until fully healed.
The goal of treatment is to keep the pain low while promoting epithelial healing.
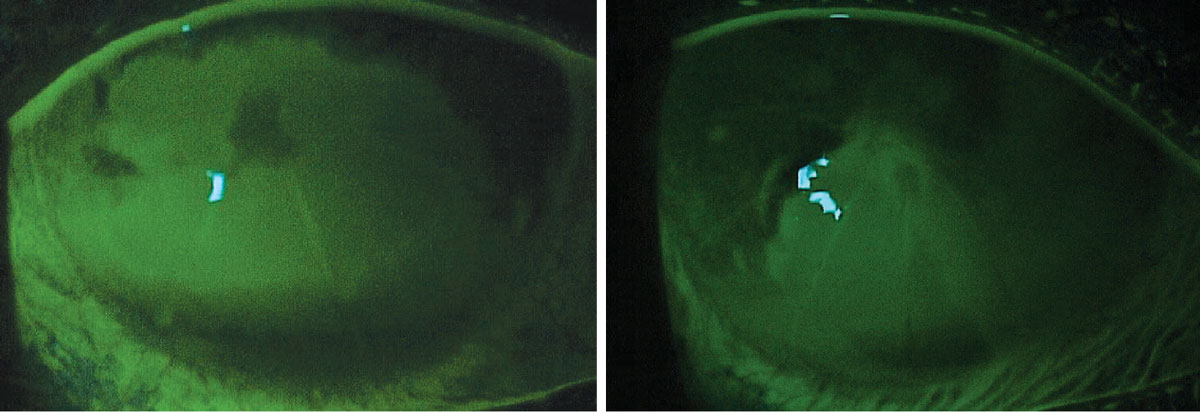 |
Fig. 3. Bilateral corneal injury from exposure to Simple Green household cleaner after instillation of sodium fluorescein dye. This patient previously had a radial keratotomy procedure. Photo: Leslie Cecil, OD. Click image to enlarge. |
Takeaways
Due to the cornea’s role in protecting the eye, it is commonly injured in trauma, resulting from a multitude of etiologies as discussed. With prompt care and treatment, these conditions can be managed and visual acuity can be preserved.
1. Aslam SA, Sheth HG, Vaughan AJ. Emergency management of corneal injuries. Injury. 2007;38(5):594-7. 2. National Society to Prevent Blindness. Operational research Department. Vision problems in the US. New York: The Society. 1980. 3. Willmann D, Fu L, Melanson SW. Corneal injury. In: StatPearls. Treasure Island (FL). July 18, 2022. 4. Ljubimov AV, Saghizadeh M. Progress in corneal wound healing. Prog Retin Eye Res. 2015;49:17-45. 5. Kamil S, Mohan RR. Corneal stromal wound healing: Major regulators and therapeutic targets. Ocul Surf. 2021;19:290-306. 6. Surgical management of anterior segment trauma. In: Krachmer J, Holland E, Mannis M, eds. Cornea. Chicago: Mosby-Year Book, Inc., 1997. Accessed March 20, 2023. 7. Macsai MS. The management of corneal trauma: advances in the past twenty-five years. Cornea. 2000;19(5):617-24. 8. McGrath LA, Lee GA. Techniques, indications and complications of corneal debridement. Surv Ophthalmol. 2014;59(1):47-63. 9. Yu CW, Kirubarajan A, Yau M, et al. Topical pain control for corneal abrasions: a systematic review and meta-analysis. Acad Emerg Med. 2021;28(8):890-908. 10. Kaiser PK. A comparison of pressure patching versus no patching for corneal abrasions due to trauma or foreign body removal. Corneal Abrasion Patching Study Group. Ophthalmology. 1995;102(12):1936-42. 11. Wipperman JL, Dorsch JN. Evaluation and management of corneal abrasions. Am Fam Physician. 2013;87(2):114-20. 12. Welch, L., Hunting, K., Mawudeku, A. Injury surveillance in construction: eye injuries. Appl Occup Environ Hyg. 2001;16:755-62. 13. Singh P, Tyagi M, Kumar Y, et al. Ocular chemical injuries and their management. Oman J Ophthalmol. 2013;6(2):83-6. 14. Hemmati H, Colby K. Treating acute chemical injuries of the cornea. Am Acad Ophthalmol. 2012;43-5. 15. Welch L, Hunting K, Mawudeku A. Injury surveillance in construction: eye injuries. Appl Occup Environ Hyg. 2001;16(7):755-62. |