 |
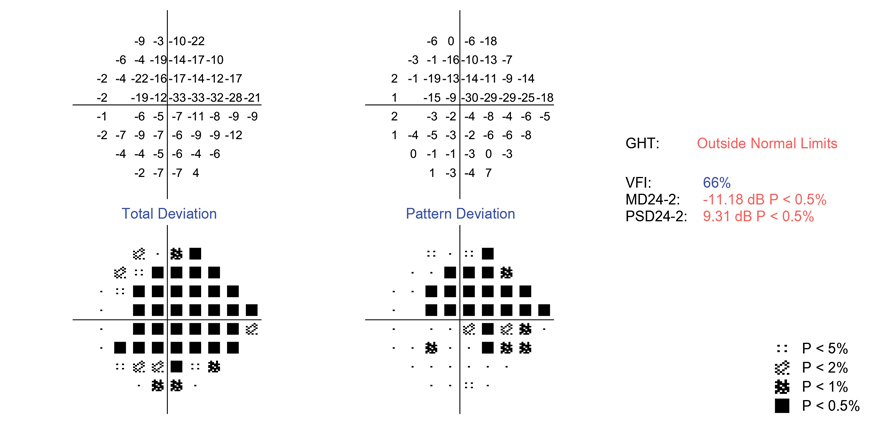
| Greater visual field loss at baseline, lower baseline IOP, existing POAG and use of a lower number of baseline topical glaucoma agents in the fellow eye were found to be predictors of treatment failure with topical glaucoma medication. Photo: Danica Marrelli, OD. Click image to enlarge. |
Despite increased acceptance of SLT as a first-line option in glaucoma care, the most common initial intervention remains topical IOP-lowering agents, as pressure is the most important modifiable risk factor for development and progression of primary open-angle glaucoma (POAG). However, continued maintenance of adequate IOP control with medical therapy often requires treatment intensification, which undermines on adherence, so British researchers recently aimed to assess treatment success duration when administering topical glaucoma drugs.
Five years of medical records were extracted from five secondary-care and tertiary-care UK ophthalmology centers and examined for initiating/intensifying topical glaucoma medication patterns. Main study outcomes were time from treatment initiation/intensification to treatment failure (defined here as <20% IOP reduction or IOP >21mm Hg at consecutive clinic visits, or intensification of glaucoma treatment) and time from treatment change to subsequent treatment intensification.
A total of 6,587 eyes were included in the study, published recently in British Journal of Ophthalmology, and a total of 7,684 treatment events were noted. Of these, 69.7% were initiation of treatment, 19.1% represented escalation from one to two drops and the remaining 11.2% of events concerned patients who added a third drop. Median time to treatment failure was 1.60, 1.00 and 0.92 years, respectively, following each of these treatment decisions (treatment initiation, adding a second drop, adding a third). Median time to treatment intensification was 4.68 years for treatment initiators, 3.83 years for escalation to two drops and 4.35 years for adding a third.
This study identified greater visual field loss at baseline, lower baseline IOP, existing POAG and use of a lower number of baseline topical glaucoma agents in the fellow eye as predictors of treatment failure with topical glaucoma medication.
“The association between lower baseline IOP and treatment failure may be related to the difficulty of achieving and maintaining ≥20% IOP reduction in eyes with pre-existing low IOP. In contrast, lower baseline IOP was protective against treatment escalation,” the authors explained in their BJO paper.
Patients remained on their index therapy for a median of 3.8 to 4.7 years, yet the median time to onset of inadequate IOP-lowering effect was 0.9 to 1.6 years. This lag exceeds that reported in other studies, the authors noted.
“At first glance, this implies a delay between clinical indication and escalation, highlighting a window of opportunity for clinical review and intervention. However, there are considerations other than IOP—both clinical and patient-related factors—that inform the treatment escalation decision in the context of long-term disease management,” the authors explained. Examples include a switch to another topical med, the delaying effects of patient non-adherence and risk/benefit concerns among clinicians about adding another drop to the regimen.
Fu DJ, Ademisoye E, Shih V, et al. Survival of medical treatment success in primary open-angle glaucoma and ocular hypertension. Br J Ophthalmol. April 6, 2024. [Epub ahead of print.] |