 |
Q: Even though contact lens designs and materials have improved, the rate of corneal infection in wearers hasn’t changed in over two decades. What are the most common causes of infection? How can we limit them? Are there any barriers?
A: “The ocular surface is resilient to infectious events,” according to optometrists Mile Brujic and David Kading, who practice in Ohio and Washington, respectively. However, it is not immune to infection. Contact lens abuse can challenge the ocular surface and increase a patient’s chance of developing microbial keratitis.
Interestingly, there is a difference in pathogens between corneal infections that are secondary to contact lens wear vs. those that are not. A recent study demonstrated that the causative pathogen in cultured contact lens-related ulcers was predominately Pseudomonas species (44%), followed by gram-positive (33%) organisms, fungi (13%), other gram-negative (6%) bacteria and Acanthamoeba (5%).1 Cultured non-contact lens-related ulcers were primarily caused by gram-positive (64%) and gram-negative (26%) organisms, as well as fungi (11%).1
Among the many risk factors, overnight wear of contact lenses and failure to wash and dry hands prior to lens insertion are known to increase the chance of infection. Poor storage hygiene also increases the risk of infectious keratitis. The lens modality is another important factor and can influence corneal infection, with the lowest risk of severe disease occurring in daily disposable and rigid gas permeable lens wearers.2
Infection Origins
 |
|
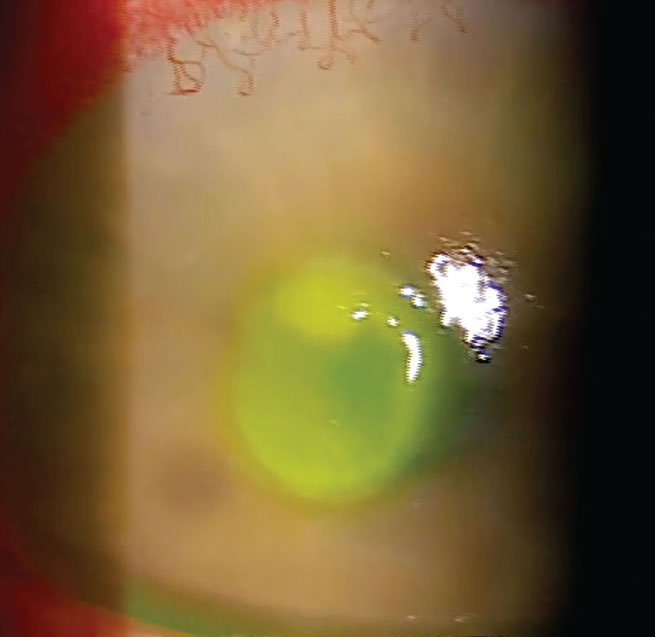
Central corneal ulcer secondary to contact lens abuse. Click image to enlarge. |
Understanding there are risk factors that are modifiable and conveying them to patients is critical to ensure contact lens success and avoid corneal infection, Drs. Brujic and Kading note. Continuous lens wear through the day and overnight creates the greatest risk of corneal infection. Educating patients on the destructive nature of this habit and helping them steer clear of it makes a world of difference in ocular health.
Upon determining an appropriate wear schedule, patients must learn how to properly wash and dry their hands prior to lens handling to avoid introducing any harmful substances into the ocular environment. For the same reason, appropriately cleaning and replacing the case and storing the lenses is equally as important. This last risk factor can be mitigated by prescribing options that eliminate the need for storage cases, such as daily disposable lenses, as long as they are available in the patient’s prescription and able to be prescribed. This modality also takes overnight wear out of the equation.
Patient Hurdles
Of course, patient compliance presents a challenge—even when the stakes are as high as the potential for risk of corneal infection, Drs. Brujic and Kading say. While this is a factor we can’t control once the lens is dispensed and the patient leaves our office, it is one we can attempt to influence. Although daily disposables reduce the risk of disease, some patients may not be able to pursue this modality due to financial restrictions or prescription unavailability. As a result, the lenses they are prescribed require the use of a case for storage and sanitation purposes.
While appropriate patient and lens hygiene may seem easy, this part of the process is often the most neglected by patients. Offer clear and concise education on the steps patients should take. If they fail to follow your advice, consequences will come into play.
Clinical Takeaways
Corneal infection is destructive, but also avoidable in most cases of contact lens wear. Educating ourselves on how to appropriately manage any relevant risk factors and then passing on our knowledge to our patients is key. By doing our part, we’ve given our patients the tools they need to do it on their own.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Bennett L, Hsu HY, Tai S, et al. Contact lens versus non-contact lens-related corneal ulcers at an academic center. Eye Contact Lens. 2019;45(5):301-5. 2. Stapleton F. Contact lens-related corneal infection in Australia. Clin Exp Optom. 2020;103(4):408-17. |

