Many people have seen a video of a young child seeing their parents’ faces clearly after putting on glasses for the first time. That first look of surprise is often followed with a smile that could melt your heart. That specific opportunity is few and far between, but there are still many other rewarding aspects of serving our pediatric patients. An eye examination of your adult patients should differ from the eye examination of your pediatric patients. Visual skills and ability are developed during childhood, and the eye examination should mirror the developmental ability of the child. Remember that the chronologic age of a child may not equal their developmental ability. As children grow, so do their visual skills and demands.
 |
| Click image to enlarge. |
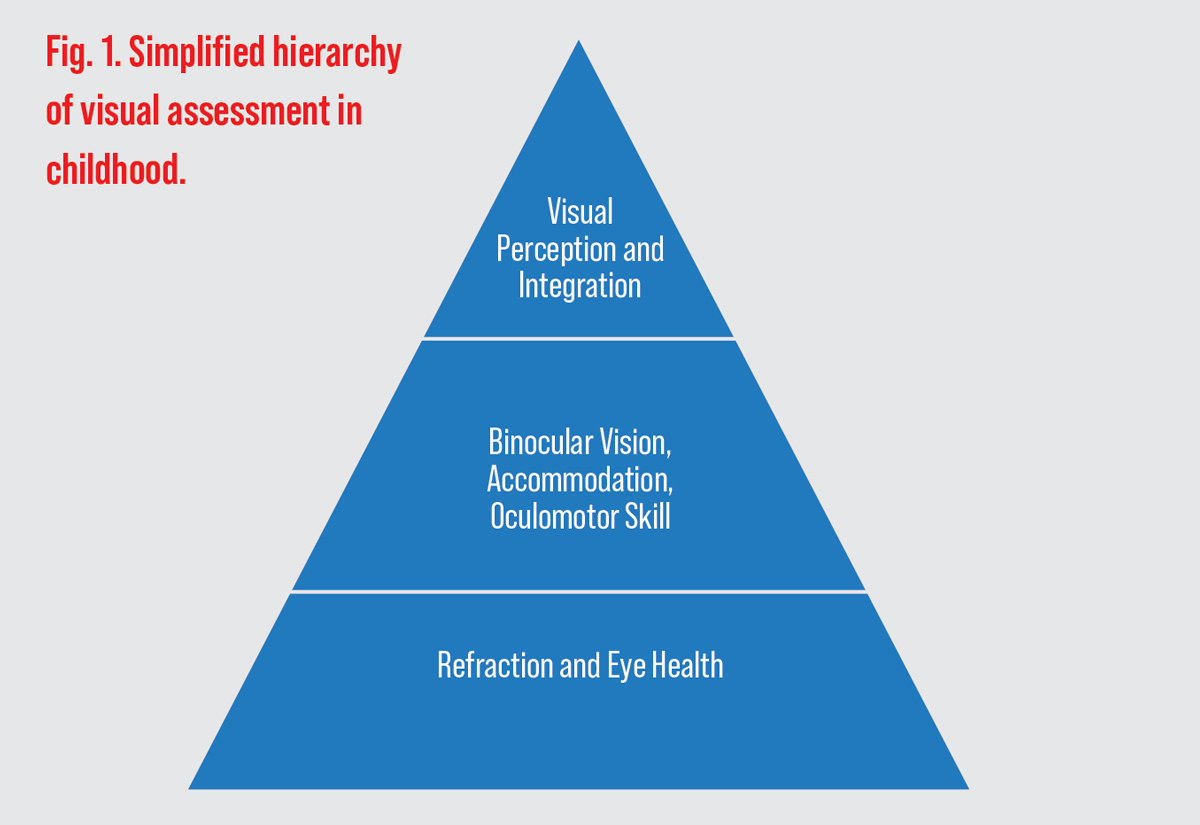
The eye examination of a toddler should be distinguished from the visual assessment of a primary school-aged child. Visual skills are built upon the foundation of healthy eyes and adequate visual acuity (VA), which is where we should start with our infant examinations (Figure 1). The first eye examination should take place between six and 12 months of age. If there are no concerns, then the second eye examination should take place at three years of age and then at five years of age and on an annual basis thereafter. This article will discuss how to conduct an easy pediatric exam and relay findings with parents.
Not Just Small Adults
Keep in mind that the visual demands of a child are different from those for adults. Children learn through tactile and motor activities for the first few years of life. Those activities rely more heavily on visual perception and visual motor integration than the ability to see letters on an acuity chart.1
When performing eye exams in pediatric patients, it is crucial to evaluate for any presence of disease. With that said, the most common ocular morbidities in childhood are refractive error and strabismus.2,3 This article will emphasize the vast majority of childhood findings and not disease itself.
 |
| Click table to enlarge. |
Let’s consider visual considerations through childhood:
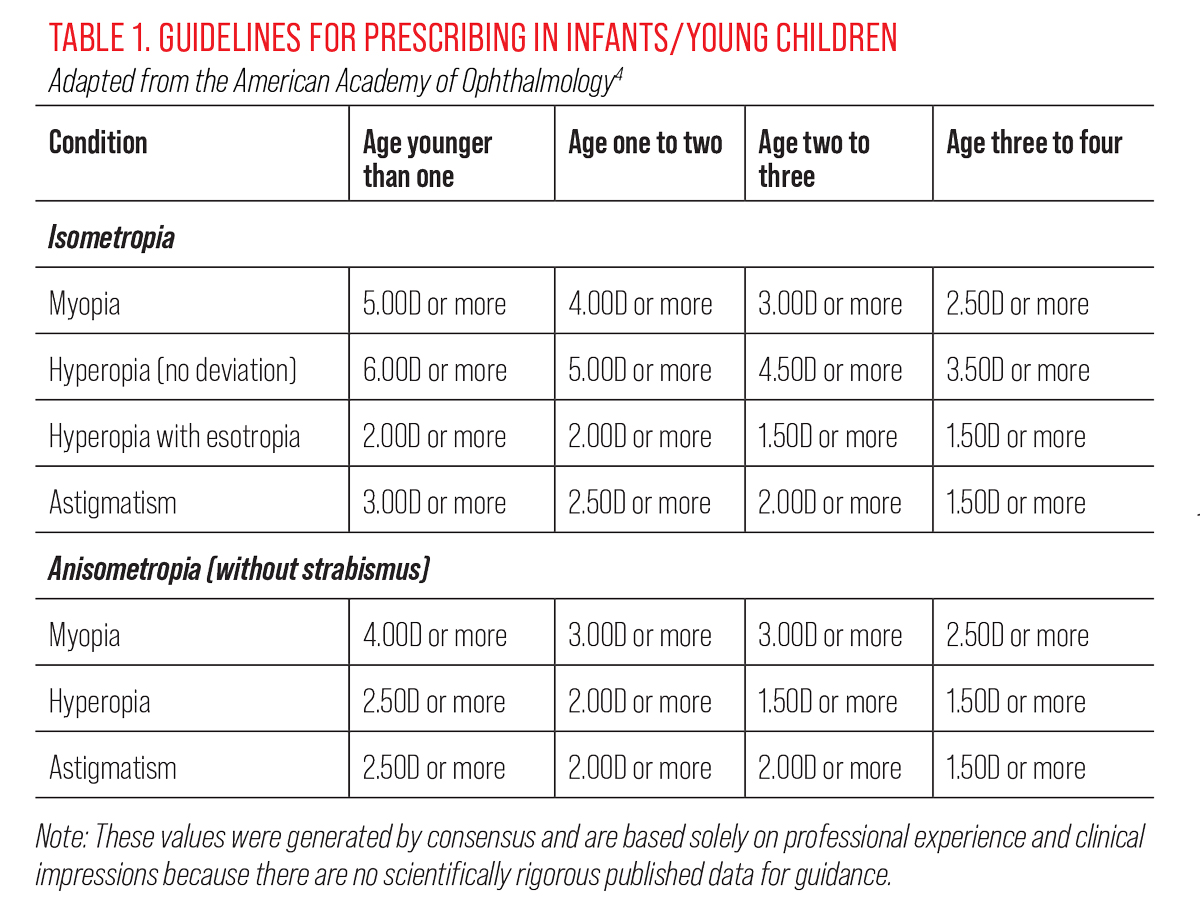
Infancy to age three. In early life, children learn through tactile exploration. Most of their visual demands will be within a few feet from their face. Motor development is the foundation for vision development, which then guides increasingly complex motor skills. Adequate binocular vision, accommodation and accurate eye movements are important for children to reach their potential with motor skills and spatial awareness. Refractive findings are relevant when they are amblyogenic or when presenting with a strabismus; otherwise, allow emmetropization to occur and watch patients carefully with borderline refractive findings (Table 1).4 In this age group, it is recommended to attempt to measure VA as a later step in the examination. A sample can be found in “Suggested Exam Flow for the Infant/Toddler.”
Ages three to six. Much learning should still occur through tactile and motor stimulation, but children in this age group are starting to use their vision and perceptual skills for more reading-based learning purposes.1 As children enter the classroom, adequate distance and near VA are necessary to meet the expected classroom environmental demands. Assess near vision and binocular status to ensure the child has the visual skills to learn to read in such a pivotal time of their development.
Ages seven to 14+. At this point in education, children move from the “learning to read” phase into the “reading to learn” phase. Efficient visual skills aid in the development of reading ability and are an important piece of development for further educational progress. In this age group, subjective findings are typically much easier to collect and best-corrected VA can be more accurately measured. This is often when binocular dysfunctions present with symptoms as the visual demands increase to a level that requires sustained visual efficiency.
Suggested Exam Flow for the Infant/Toddler
|
Ask the Right Questions
Most parents are unaware of the link between vision and performance/learning. Their understanding of an eye examination is to determine the need for glasses/contact lenses to aid VA. Many are surprised to hear that there is much more to a comprehensive vision examination that evaluates a child’s ability to meet the demands of the classroom. It is our job to probe the parent and child for clues that may warrant an extended visual evaluation.
Here are sample history questions to ask the child’s parent/caregiver:
• Was the child born full-term? If not, what was the length of gestation and how much did they weigh at birth? Children born prematurely with lower birth weight are at an increased risk of developmental delay including visual delays.5
• Did they reach all developmental milestones on time? Visual problems are more common in children with delayed developmental milestones.5
Here are sample performance questions to ask the parent of a school-aged child:
• Is your child reading at an appropriate age level? Vision may impact reading skills, and if this question is answered in the affirmative, then consider additional visual testing beyond a routine eye examination.6
• Does your child struggle with reading but excel in other subjects? Vision problems such as convergence insufficiency, accommodative dysfunction and oculomotor dysfunction tend to cause a struggle in subjects that incorporate a higher reading demand compared with other subjects.
• Do you feel as though your child is reaching their full potential? A gap in potential may indicate a visual processing disorder. “A high verbal IQ combined with a performance IQ that is 20 points lower should signal the need for an optometric evaluation,” says Linda Kreger Silverman, PhD.7
• Does your child avoid reading-related tasks? Visual symptoms may not be present if the child simply avoids extended near point tasks such as reading.
• Is there a concern or diagnosis of attention deficit hyperactivity disorder? Attention disorders are more common in children with visual dysfunction.8
Here are sample questions to ask the school-aged child:
• What is your favorite subject in school? What is your least favorite subject? Children who dislike subjects heavy in reading are more likely to have vision problems compared with students who favor subjects heavy in reading.
• Do you ever see the words moving on a page when you are trying to read?
• Do you ever see two of things when you’re looking at them?
• Do your eyes or head hurt after looking at something?
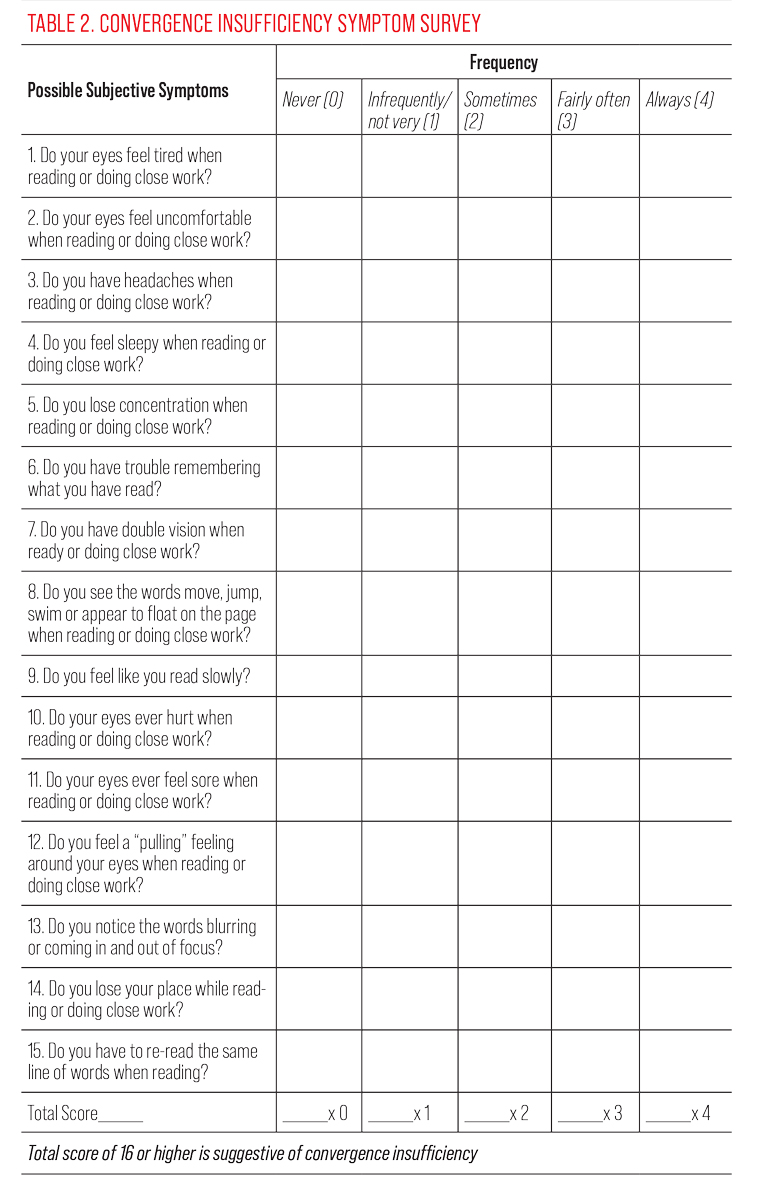
If the history questions suggest that a child has a vision problem, then it is helpful to quantify the symptoms. The Convergence Insufficiency Symptom Survey (CISS) is a 15-item questionnaire that has a 96% sensitivity and 88% specificity at identifying children with convergence insufficiency when using >16 as a cutoff score (Table 2).9 The CISS also identifies children with disorders other than convergence insufficiency that interfere with comfortable near visual function.10
 |
| Click table to enlarge. |
If a child has an identifiable complaint, ask for the familiar features regarding the symptom such as onset, location, duration, character, aggravating and associated factors, relieving factors, timing and severity of symptoms. If there are asthenopia complaints in the frontal region of the head that occur more frequently in the afternoon compared with first waking, suspect a vision problem until ruled out by extensive visual testing. If you do not have any findings to explain the child’s complaints during the time of the eye examination, then perform additional visual evaluation or refer to a colleague who does (locate.covd.org). That testing should include a complete binocular and accommodative evaluation and may include a cycloplegic refraction. In the past, the timing of symptoms during the academic week compared with the weekend would be a meaningful history question to differentiate symptoms emanating from a vision problem. With the ubiquitous nature of near point screen use, we are not so quick to dismiss a vision problem when symptoms are equal on school days compared with non-school days.
 |
|
Fig. 2. Near fixation targets. Click image to enlarge. |
Clinical Testing
An excellent starting point for determining what testing is appropriate for pediatric patients can be found in the American Optometric Association’s evidence-based clinical practice guideline, “Comprehensive Pediatric Eye and Vision Examination.”10 However, each child brings a unique combination of language development, cognitive function, comfort level and attention in the exam room that may make standardized testing challenging. Keep your testing options open and flexible based on the individual in order to gather enough data to inform your clinical decisions. A helpful strategy is to start with the known testing standard for each exam element and modify accordingly if the child cannot accurately perform or sit for the test.
Refraction. For children who may have difficulty with subjective responses, rely on your retinoscope. A computer/laptop in the exam room is very helpful with obtaining retinoscopy findings. Videos of interest are easily accessible through a web search and help to hold a child’s visual attention. If you plan on prescribing lenses, it is recommended to trial frame the retinoscopy findings and check VA. In the case of a child who has difficulty with subjective responses, rely on the observable responses to the lenses including the quality of the retinoscopy reflex and any improvement in fixation/visual attention. Due to active accommodation and poor fixation, non-cycloplegic autorefractor measurements are often unreliable. Cycloplegic auto-refraction is more reliable than non-cycloplegic findings. It is not recommended to prescribe solely based on autorefractor findings. Whether performed under cycloplegia or not, the results do not elucidate how a child is functioning in their habitual state including the impact of their binocular vision and accommodation.
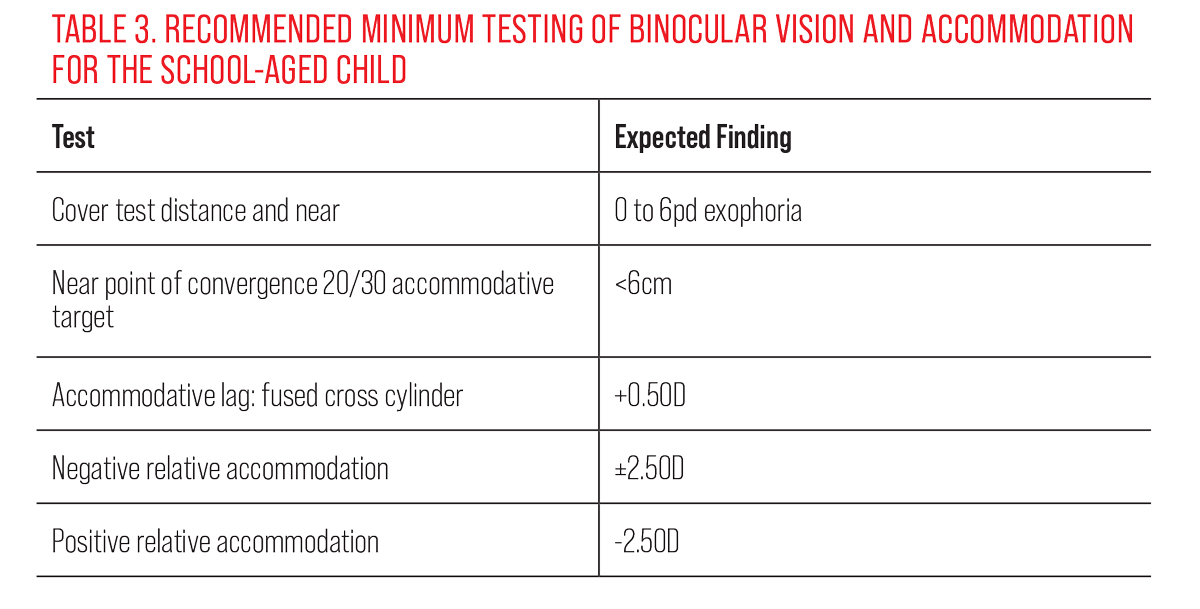
Binocular/accommodative/oculomotor. It is important to have engaging fixation targets for young children. Spinning light wands are an effective fixation target to assess extraocular muscle movement. Light up animal keychains have proven to be effective at drawing a child’s visual attention. Younger children should be engaged in a target of interest while using your thumb to perform the cover test. For the uncooperative child, binocular status can be estimated via the Hirshberg reflex. Older children should be instructed to look at a 20/30 size VA target (or two lines above best VA) for binocular and accommodative evaluation (Figure 2). Minimum recommended testing and expected findings during a “routine” eye examination for the school age child can be found in Table 3.
 |
| Click table to enlarge. |
Stereoacuity. Stereopsis is an important indicator in the development of normal binocular vision. For preschool-aged children, the Preschool Assessment of Stereopsis with a Smile (PASS) test is recommended for random dot stereoacuity testing. At later ages, perform the Randot stereoacuity test, which offers both global targets which require bifoveal fixation and local stereoacuity measurements.
Anterior segment. For broad assessment in the young child, a 20D lens can be used as a magnifier with a light source, such as a penlight. This can help identify any ocular disease associated with the lids, lashes and conjunctiva, as well as allow gross assessment of the cornea, iris and lens. If fluorescein evaluation of the cornea is warranted, a useful tool is an owl light up keychain that incorporates blue LED lights (Figure 3).
Posterior segment. Most disease of this area in pediatric patients is found in the posterior pole. If a peripheral evaluation is difficult based on the patient’s attention and fixation, getting a clear look at the optic nerve and macula can suffice. A direct ophthalmoscope can be used with a 20D lens to get a full view of the posterior pole. Using the lens as you would for indirect ophthalmoscopy, focus the direct ophthalmoscope to the lens by dialing in approximately +3 and tromboning the lens until it’s full of light. With enough practice, this can be done on undilated pupils as well.
VA. Measuring acuity in preschool aged children can be accomplished using HOTV or LEA symbols. If a child has a hard time recognizing a shape or is shy in the exam room, a matching chart can be given. VA does not only test for the threshold of eyesight. Performing these tests requires visual skills including fixation, attention and discrimination. In younger children, we typically reach the threshold of visual perception before reaching the threshold of VA. Therefore, it is not uncommon nor an indication of any deficit when the child does not see 20/20 VA.
Qualitatively, pay attention to whether the child is resistant to occlusion of one eye. If a child gets upset or quiet with occlusion or if they actively try to duck away from occlusion, it may be an indicator that the uncovered eye has reduced acuity. While this is not a standard measurement of VA, it is an important clinical finding that should be noted in the patient’s chart. If the VA cannot be measured but the patient has an amblyogenic factor, this simple observation may guide your treatment plan.
 |
|
Fig. 3. A blue LED owl keychain can be useful for corneal assessment. Click image to enlarge. |
Make a Diagnosis
The most common visual diagnoses outside of ametropia are amblyopia and non-strabismic binocular vision problems. There have been exciting new developments in amblyopia treatment of late. Amblyopia is found in 3% of pediatric patients and carries with it a significant public health concern. Amblyopia is a neurodevelopmental disorder in which binocular visual development is disrupted. While this often manifests with monocular findings, such as reduced VA, oculomotor abnormalities and reduced accommodative function in the delayed eye, amblyopia is a binocular vision problem at its core. Restoring binocular function is emerging as an alternative to the centuries-old treatment of monocular patching. Monocular patching has poor compliance, reported at 40% along with a 25% recurrence of amblyopia once patching is discontinued.11 Patching does not address the neurologic basis of the disease. The modernized approach to anisometropic amblyopia management is to minimize binocular competition to maximize overall visual performance.12
The Sanet-Vergara treatment protocol recommends prescribing the combination of refractive powers that provides the best binocular response through Worth 4 Dot and stereopsis testing at distance and near. This often means reducing the refractive power of the amblyogenic eye to allow better sensory fusion and, thus, treats the amblyopia through the binocular system. If occlusion therapy is necessary, translucent occlusion with Bangerter filters may be used. This will facilitate binocular integration and allows for adjustments in the degree of occlusion as the condition improves.13 The standard of care in the treatment of amblyopia will likely shift from monocular patching to binocular treatment in the near future.
Non-strabismic binocular vision problems include disorders of vergence and accommodation. The most common of these diagnoses is convergence insufficiency (CI).14 The textbook definition of CI includes exophoria at near greater than distance, receded near point of convergence (NPC) and reduced positive fusional vergence (PFV). There are patients who “do not read the textbook” and present with CI without all of the classically expected findings. Patients may have esophoria at near and CI as they have a receded near point of convergence.15
The patient with CI may be able to pass the NPC test on the first attempt only to show a receded NPC on repeat testing. The patient with CI may have a normal NPC but reduced PFV findings. It may be difficult to properly diagnose CI within the time constraints of an annual eye examination. Therefore, it is crucial to ask about the common signs and symptoms of binocular and accommodative dysfunction during the examination, and if present, schedule or refer the patient for further visual testing.
Takeaways
Providing comprehensive pediatric vision care is an excellent way to build a practice and is rewarding for both the patient and doctor. Diagnosing road blocks in vision development including ametropia, binocular vision dysfunction, accommodative dysfunction, oculomotor dysfunction, amblyopia and strabismus is an important step for children to receive full-scope care. Treatment may include lenses, prisms and/or optometric vision therapy. Successful treatment of the vision problem, whether in your practice or referred to a colleague, helps the child reach their full potential and creates a lifetime of gratitude for the diagnosing doctor. We are grateful to be in a position to make such a positive impact on the lives of children.
Dr. Press practices at Park Ridge Vision and is board-certified in vision development and therapy. He is a fellow of the College of Optometrists in Vision Development and is an advisory board member for Review of Myopia Management. Dr. Press is a paid consultant for Johnson & Johnson Vision.
Dr. Cohen practices at Park Ridge Vision. She is a fellow of the American Academy of Optometry, as well as a member of the Illinois Optometric Association, the American Optometric Association and the College of Optometrists in Vision Development. She has no financial disclosures.
1. Oberer N, Gashaj V, Roebers CM. Executive functions, visual-motor coordination, physical fitness and academic achievement: Longitudinal relations in typically developing children. Hum Mov Sci. 2018;58:69-79. 2. Kelkar J, Kelkar A, Thakur P, Jain HH, Kelkar S. The epidemiology and disease pattern of pediatric ocular morbidities in Western India: The National Institute of OphthalMology AmBlyopia StUdy in Indian Paediatric EyeS (NIMBUS) study report 1. Indian J Ophthalmol 2023;71(3):941-5. 3. Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295(18):2158-63. 4. Braverman RS. Types of amblyopia. American Academy of Ophthalmology. www.aao.org/education/disease-review/types-of-amblyopia. October 21, 2015. Accessed April 15, 2023. 5. Soleimani F, Zaheri F, Abdi F. Long-term neurodevelopmental outcomes after preterm birth. Iran Red Crescent Med J. 2014;16(6):e17965. 6. Quaid P, Simpson T. Association between reading speed, cycloplegic refractive error and oculomotor function in reading disabled children vs. controls. Graefes Arch Clin Exp Ophthalmol. 2013;251(1):169-87. 7. Kay K, ed. Uniquely Gifted: Identifying and Meeting the Needs of Twice Exceptional Learners. Avocus Publishing; 2000:153-65. 8. Granet DB, Gomi CF, Ventura R, Miller-Scholte A. The relationship between convergence insufficiency and ADHD. Strabismus. 2005;13(4):163-8. 9. Borsting EJ, Rouse MW, Mitchell GL, et al.; Convergence Insufficiency Treatment Trial Group. Validity and reliability of the revised convergence insufficiency symptom survey in children aged nine to 18 years. Optom Vis Sci. 2003;80(12):832-8. 10. Horan LA, Ticho BH, Khammar AJ, et al. Is the Convergence Insufficiency Symptom Survey Specific for convergence insufficiency? a prospective, randomized study. Am Orthopt J. 2015;65:99-103 11. American Optometric Association. Evidence-based clinical practice guideline: comprehensive pediatric eye and vision examination. Optometric Clinical Practice. 2020. www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/EBO%20Guidelines/Comprehensive%20Pediatric%20Eye%20and%20Vision%20Exam.pdf. Accessed April 15, 2023. 12. Wygnanski-Jaffe T, Kushner BJ, Moshkovitz A, et al; CureSight Pivotal Trial Group. An eye-tracking-based dichoptic home treatment for amblyopia: a multicenter randomized clinical trial. Ophthalmology. 2023;130(3):274-85. 13. Giménez PV, Sanet R, Press L, et al. Management of anisometropic amblyopia: a retrospective study. Vis Dev Rehabil. 2023;9(1):32-40. 14. Scheiman M, Kulp MT, Cotter SA, et al. Interventions for convergence insufficiency: a network meta‐analysis. Cochrane Database Syst Rev. 2020;12(12):CD006768. 15. Rafif Ghadban, Jennifer M. Martinez, Nancy N. Diehl, Brian G. Mohney, The incidence and clinical characteristics of adult-onset convergence insufficiency. Ophthalmology. 2015;122(5):1056-9. |

