 |
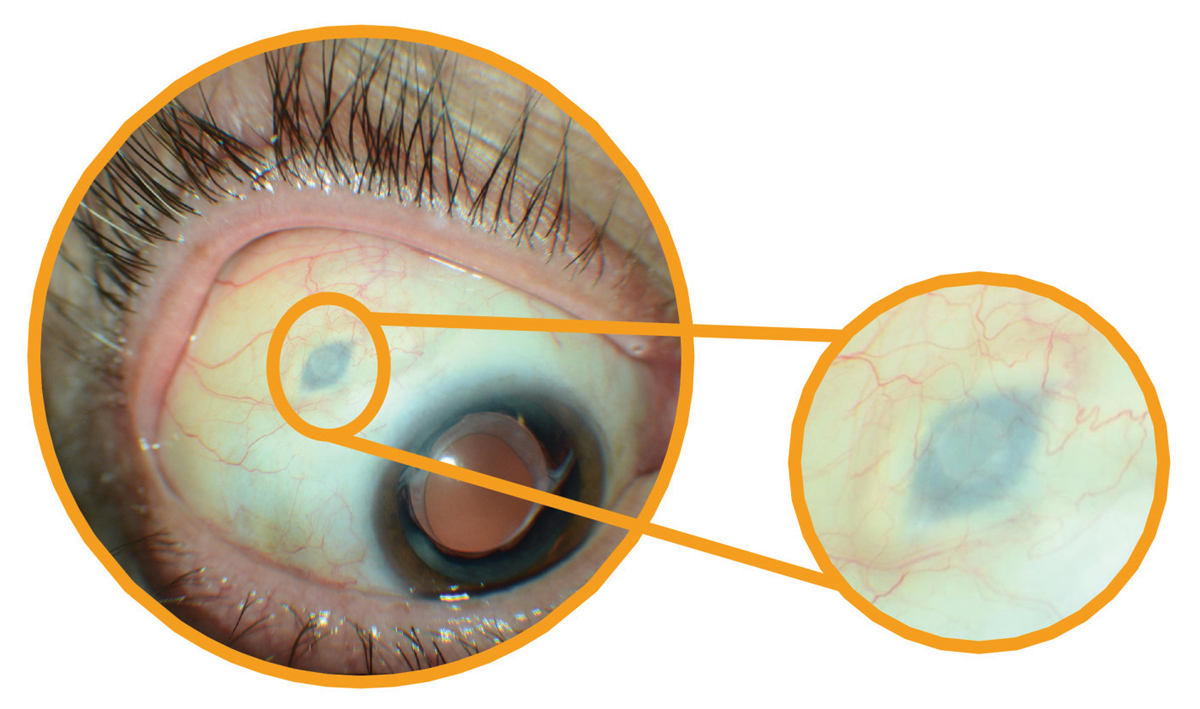
| The Susvimo implant, pictured here, is one of the newest innovations in anti-VEGF delivery for AMD treatment. Photo: Anat Loewenstein, MD. Click image to enlarge. |
After a few years of celebration over having an effective therapy for wet AMD in the form of intravitreal anti-VEGF injection—itself a game-changer—researchers quickly turned their attention to the goal of reducing patients’ treatment burden, as a monthly regimen of anti-VEGF injections was unstainable on many fronts. Drugs with increased duration of effect, like Eylea and more recently Vabysmo, certainly helped, as did “treat-and-extend” care regimens. The biggest recent gain came last year with the FDA approval of the Susvimo implant, formerly known as the Port Delivery System (PDS), a device that elutes ranibizumab in a controlled manner 100mg/ml over a six-month period. Susvimo reduces the number of injections patients receive, decreasing the overall burden of care, researchers suggest.
Patient satisfaction data from Susvimo’s Phase III ARCHWAY trial, recently published in JAMA Ophthalmology, revealed that, not surprisingly, patients preferred the PDS (refills every 24 weeks) over intravitreal ranibizumab injections (0.5mg every four weeks).1 The researchers reported that, at 40 weeks, almost all patients in the PDS arm preferred this treatment (93.2%) vs. previous intravitreal injections (1.3%), with 73.5% noting a strong preference for the PDS. Among patients who received concurrent fellow eye injections, 92.3% preferred the PDS. Since both delivery methods had high treatment satisfaction, the study authors concluded that the PDS is a meaningful alternative in wet AMD treatment.
However, patients and providers still have other considerations to keep in mind when deciding on a treatment. One of these isn’t a hot topic in clinical trials, and that’s cost. The PDS with fixed six-month refills over one-year costs on average over $21,000.
Using trial data and Medicare reimbursement rates for patients receiving anti-VEGF injections and the PDS, another set of researchers performed a cost analysis and found that the cost-savings potential of Susvimo with PRN refill in patients receiving regular ranibizumab or aflibercept injections depends on the number of injections and refills given.2 They determined that the mean number of injections to break even with the cost of the ranibizumab PDS with one refill was:
Ranibizumab: 10.8
Aflibercept: 9.3
Bevacizumab: 34.5
The researchers projected that the PDS with as-needed refills will reduce costs compared with intravitreal ranibizumab or aflibercept use at five years—but not at one year. Additionally, they noted that the PDS with one refill costs more than intravitreal ranibizumab or aflibercept injections if ≤11 or <10 injections, respectively, are required within the first year.
“Use of [Susvimo] will be based on other factors than cost, including safety, preferred practice and willingness to undergo a surgery with frequent clinic visits,” they concluded in their paper, also published in JAMA Ophthalmology.
1. Chang MA, Kapre A, Kaufman D, et al. Patient preference and treatment satisfaction with a Port Delivery System for ranibizumab vs intravitreal injections in patients with neovascular age-related macular degeneration: a randomized clinical trial. JAMA Ophthalmol. June 16, 2022. [Epub ahead of print]. 2. Sood S, Mandell J, Watane A, et al. Cost of ranibizumab Port Delivery System vs intravitreal injections for patients with neovascular age-related macular degeneration. JAMA Ophthalmol. June 16, 2022. [Epub ahead of print]. |


