 |
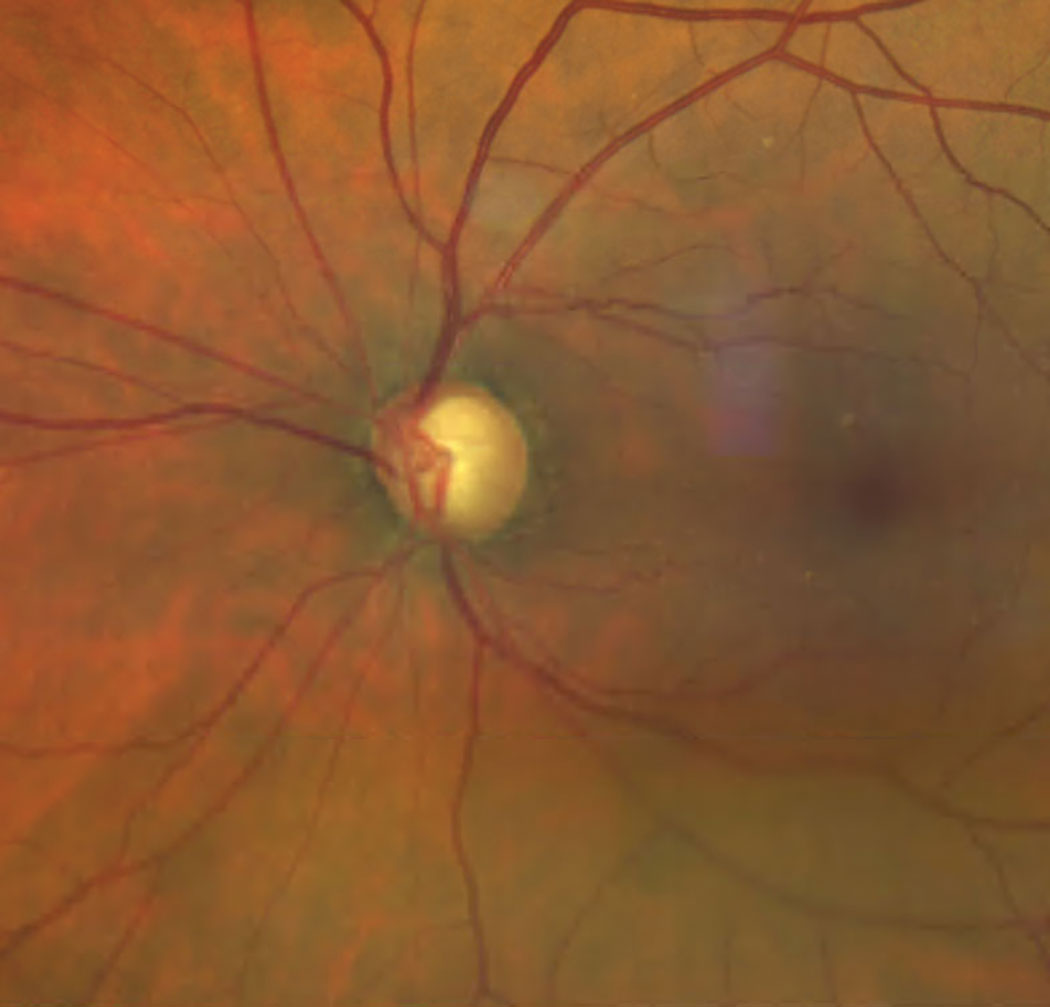
| Assessing POAG likelihood with polygenic risk score can help identify patients in need of closer monitoring due to a heightened risk of advanced disease. Photo: Bisant Labib, OD. Click image to enlarge. |
Known to be a highly heritable disease, primary open-angle glaucoma exhibits a nine-fold increased risk of development among first-degree relatives. Yet, there exists insufficient evidence on the genetic risk variants of POAG, which recently led researchers to conduct a study on the correlation between polygenic risk scores (PRS) and POAG diagnosis. Their findings confirmed that PRS identifies individuals at a substantially higher risk for POAG, supporting its increasing importance for patient risk stratification in clinical practice.
The prevalence of POAG in the highest PRS category out of 10 subgroups was more than five times the prevalence of POAG in the lowest, “indicating that those with high PRS are truly at risk of developing glaucoma,” the study authors reported in their paper, published recently in JAMA Ophthalmology.
The cross-sectional, population-based study included 407,667 participants from the UK Biobank between the ages of 40 and 69. Of these, 14,171 had a diagnosis of POAG. Using a genome-wide polygenetic risk score, researchers identified those at the highest risk of POAG and observed several associated factors after reviewing patients’ clinical data and fundus photos. These individuals demonstrated more advanced disease, including higher cup-disc ratio and intraocular pressure, thinner macula-region retinal nerve fiber and ganglion cell complex layers, greater medication requirements and a more common need for surgical intervention.
POAG PRS was also associated with a greater prevalence of disc hemorrhages and lower corneal hysteresis, the study authors reported. Thy explained in their paper that the former association may not be clinically significant due to the rarity of the event and the possible inclusion of eyes with disc hemorrhage from causes other than glaucoma. Still, they point out that “multiple studies have demonstrated a strong association between disc hemorrhage and glaucoma progression,” and that “this suggests that accumulated genetic risk burden may predispose individuals to glaucoma visual field progression.” Furthermore, they suggest, “the association between higher PRS and prevalence of disc hemorrhages may point to alternate ischemic or vascular etiology in high PRS glaucoma compared with glaucoma associated with low PRS.”
Because higher PRS was associated with lower corneal hysteresis in this study, the researchers advise clinicians to give this measurement more attention in glaucoma risk assessment. “Multiple studies have demonstrated that corneal hysteresis is strongly associated with glaucoma presence, risk of progression and effectiveness of certain treatments,” they wrote in their paper. Interestingly, they noted that “even in patients with glaucoma and well-controlled intraocular pressure, lower corneal hysteresis was associated with a higher risk of global visual field progression.”
A growing body of research, including the present study, validates the application of PRS risk stratification in identifying individuals at higher risk of complex diseases, including POAG. “Continuing to investigate the genetic markers contributing to our PRS may further our understanding of glaucoma pathology and reveal biomarkers useful for treatment development and disease monitoring,” the study authors conclude.
Sekimitsu S, Xiang D, Smith SL, et al. Deep ocular phenotyping across primary open-angle glaucoma genetic burden. JAMA Ophthalmol. August 17, 2023. [Epub ahead of print]. |

