 |
|
The study found that variation in HbA1c levels is also a detrimental factor to be addressed with diabetes patients, beyond the absolute value at any given time. Photo: Carolyn Majcher, OD. Click image to enlarge. |
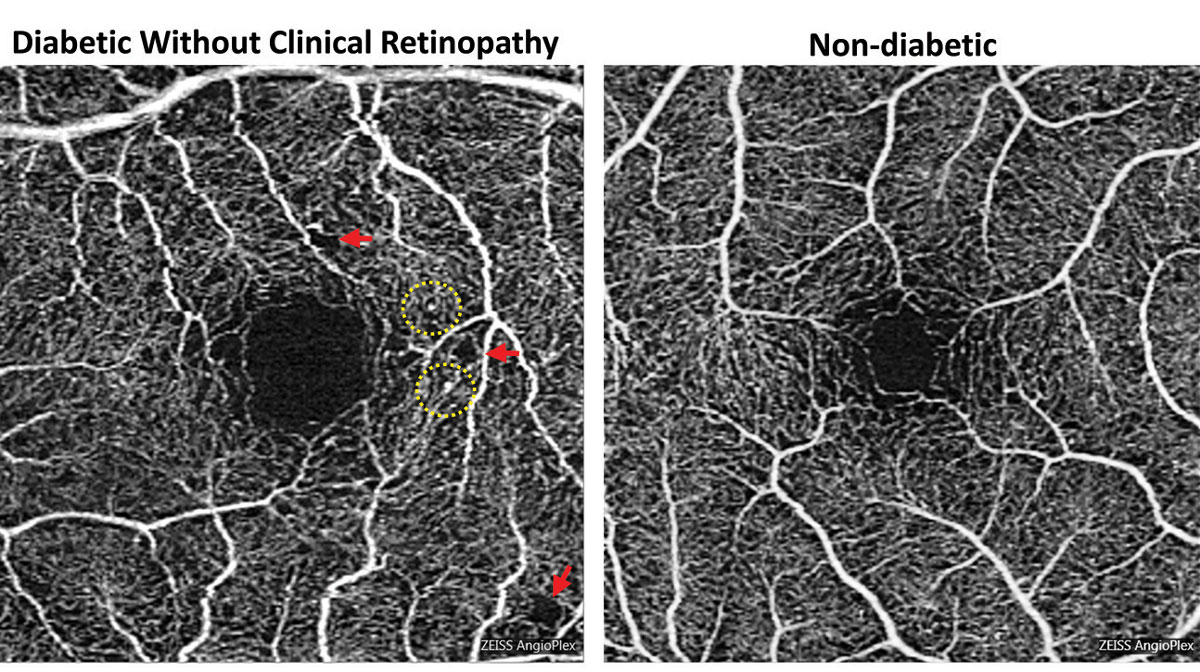
In a new study, Korean researchers investigated the association of glycemic control and retinal microvascular changes in patients with type 2 diabetes without diabetic retinopathy (DR). They found that early choriocapillaris changes on OCT angiography (OCT-A) are correlated with mean HbA1c levels and may appear prior to the onset of DR.
This retrospective study included 259 eyes of 259 participants: 88 diabetes patients with good glycemic control (mean HbA1c ≤7.0%), 81 diabetes patients with moderate control (mean HbA1c >7.0%) and 90 subjects without diabetes. No study subjects had a diagnosis of DR. OCT and OCT-A imaging parameters were compared between the three groups.
Early retinal microvascular changes on swept-source OCT-A were discovered and correlated significantly with the HbA1c level in both groups of diabetes patients without apparent DR. The strongest association was observed between the HbA1c level and choriocapillaris flow defects, which was significantly greater in the moderate control group than the good control group. “However, no significant differences were observed in separate retinal layer thickness between diabetes patients without clinical DR and controls, suggesting that retinal microvascular alterations in the choriocapillaris precede retinal neurodegenerative changes,” the authors explained.
Flow defects in the choriocapillaris were observed in diabetes patients without changes in other retinal macrovascular or microvascular features. “Considering that changes occur preferentially in the outer retina and choroidal vessels, changes in the choriocapillaris may be the earliest microvascular alterations in DM patients,” the researchers wrote in their paper for Diabetes & Metabolism Journal. “In addition to the alterations in the choriocapillaris, other OCT-A parameters showed statistically significant differences among our groups according to the degree of glycemic control.”
The moderate control, good control and healthy subjects groups had the largest FAZ area and smallest vessel density, in descending order; however, whereas the vessel density was significantly different between the healthy subjects and the good glycemic control group, the FAZ area was significantly different between the moderate control group and both other groups.
“In other words, perifoveal retinal capillaries were affected even in patients with good glycemic control, whereas the FAZ area was affected when blood glucose level was poorly controlled,” the journal article explained. “Given the abundant choroidal supply of the central macula, microcirculation in the FAZ area may be better preserved than that in parafoveal tissue despite damage to the choriocapillaris at an early stage.” The researchers then concluded that the enlarged FAZ area in subjects with high glycemic variability suggests that glycemic variability is as detrimental to the retinal microcirculation as prolonged poor glycemic control.
The clinical implications of these findings, the team suggested, is that “healthcare professionals should not only aim for optimal HbA1c levels, but also pay attention to minimizing glycemic variability. Achieving stable and consistent blood glucose levels through strategies such as continuous blood glucose monitoring and tailored treatment plans should be a key focus in diabetes management.”
Lee K, Lee GH, L SE, et al. Glycemic control and retinal microvascular changes in type 2 diabetes mellitus patients without clinical retinopathy. Diabetes Metab J. March 13, 2024. [Epub ahead of print]. |


