 |
|
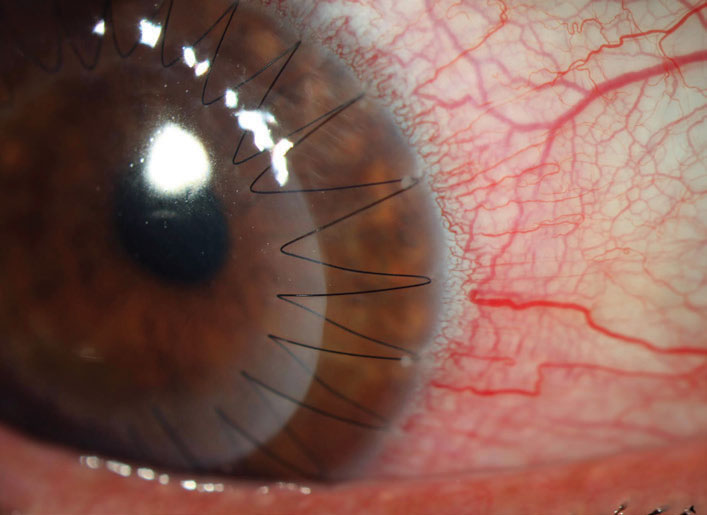
Over 70% of keratoconus patients experienced a two diopter or more increase in Kmax within five years of undergoing a PK. Photo: Aaron Bronner, OD. Click image to enlarge. |
The care of patients with keratoconus (KC) has improved dramatically in recent years, as collagen crosslinking now allows the slowing of progression early in its course. Still, some patients do progress enough eventually to require a corneal transplant. A small study published in Cornea shows that most patient who undergo penetrating keratoplasty (PK) will develop ectasia within five years.
The retrospective case series included 31 eyes of those who had a first PK and additionally had a history of KC. Since Scheimpflug imaging allows corneal ectasia diagnosis before the presentation of clinical findings or symptoms, the method is often used as a screening device to identify the condition before corneal refractive surgery. The study used this imaging modality postoperatively three months after last suture removal and subsequently performed three and five years after the PK. Postoperative graft changes after PK were determined through analyzing demographic data, donor and host trephination diameter and imaging parameters of ectasia.
The researchers found that from baseline to postoperative years three and five, the maximal keratometry (Kmax) progressed significantly. Over 70% of patients saw a Kmax increase of more than two diopters after 4.5 years and 36% saw an increase of at least 7.00D. Finding a negative correlation between host trephine size and Kmax progression, the researchers concluded that larger host trephination size is associated with smaller Kmax increase after operation. Additional changes were seen in anterior and posterior curvature of PK grafts in the KC eyes, with both exhibiting an increase in the first 4.5 years after operation.
Kmax average measurement was also steeper than the average cornea at baseline, and the researchers explain this could be due to focal areas of corneal steepening caused by anterior corneal steepening that already formed at one year after surgery, thus resulting in a Kmax increase.
With the negative correlation between host trephine size and Kmax progression, this reflects prior research finding a larger graft size resulting in better visual outcomes. For this study, the inverse relationship specifically highlights a larger host trephination diameter to be connected to less instances of postoperative ectasia, making a larger graft size advantageous to KC eyes.
Even further, research also indicates that reducing the disparity between recipient-donor trephine can decrease myopia for keratoconus patients after a PK. However, this study found that smaller graft diameter caused flatter curvature and more topographic irregularities, thus having to strike a balance between both ends.
To elucidate the main takeaway for practitioners, the authors note that “most of the KC eyes demonstrate ectatic changes within the first five years after PK, thus earlier than previously reported. Future long-term studies are needed to determine whether the ectatic changes observed by tomography precede clinical findings consistent with recurrence of ectasia in the PK grafts of eyes with KC.”
Miura M, Leon P, Nahum Y, et al. Recurrent keratoconus: Corneal transplants for keratoconus develop tomographic ectatic changes. Cornea. 2022. [Epub ahead of print]. |


