 |
|
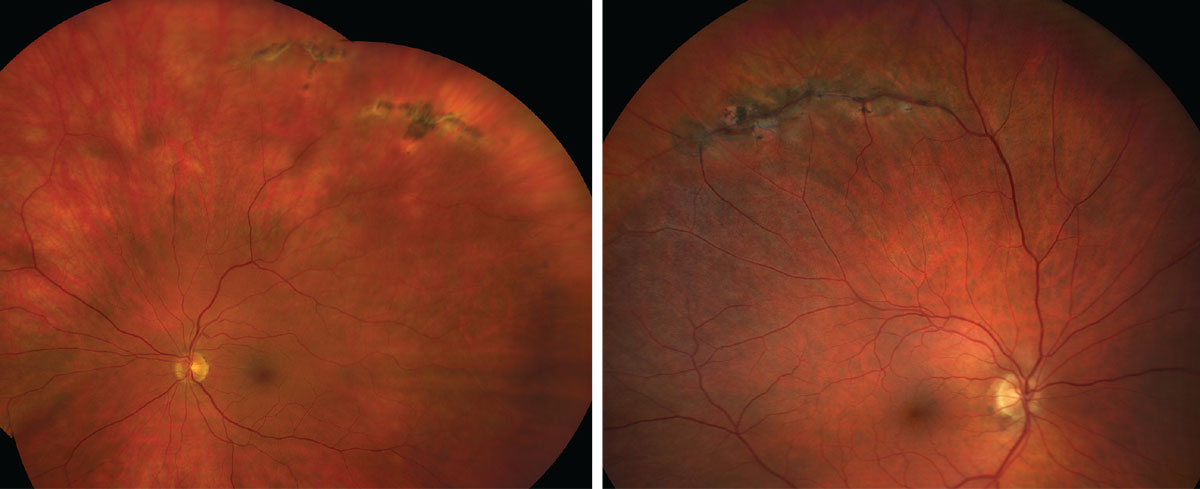
Nearly half of all eyes that develop lattice degeneration following PVD went on to develop some sort of complication, study finds. Photo: Jay M. Haynie, OD. Click image to enlarge. |
With 25% of acute symptomatic posterior vitreous detachments (PVDs) complicated by vitreous hemorrhage, retinal break or retinal detachment at initial exam or within six months of diagnosis, PVD represents a major risk for retinal complications. In a recent study, investigators aimed to examine the incidence of complications following PVD through an extended follow-up period and to identify patient-specific factors associated with greater incidence of complication.
A total of 9,635 eyes with acute PVDs between 2015 and 2019 were included. Complications (vitreous hemorrhage, retinal break and retinal detachment) were evaluated following acute PVD at presentation and throughout a six-month follow-up period.
The rate of any complication was 25%, isolated vitreous hemorrhage was 13.1%, retinal break without detachment was 16% and retinal detachment was 4.2%. The majority of each complication was noted at presentation; however, 8% of isolated vitreous hemorrhages, 19.2% of retinal breaks without detachment and 25.8% of retinal detachments were first noted within the six-month follow-up period.
Males experienced a significantly higher rate of any complication compared with females (30% vs. 21.7%), as well as retinal breaks and retinal detachments at both presentation and within the six-month follow-up. Previous studies have found males to have greater axial lengths and age-dependent increases in vitreous base width, which the authors say may play a role in the predisposition for retinal breaks and detachments among men.
Pseudophakic patients experienced significantly higher rates of delayed retinal detachment compared with phakic eyes. Among eyes with lattice/peripheral retinal degeneration, 44.2% experienced a higher rate of any complication. “The presence of retinal break in the fellow eye and retinal detachment in the fellow eye was associated with a significantly increased rate of any complication at any time point, as well as each individual complication within the six-month follow-up period,” the authors explained in their paper on the study, published in Ophthalmology.
“Prior studies have cited an approximately 10% risk of retinal detachment in the fellow eye in cases of unilateral retinal detachment,” the authors continued. “These findings are in line with observations noted in this study as we found that both a history of retinal break and retinal detachment in the fellow eye was associated with a higher risk of complication particularly within the extended six-month follow-up period.”
Among eyes with vitreous hemorrhage at presentation, 42% had a concurrent or delayed retinal break and 10.5% had concurrent or delayed retinal detachments.
“Accordingly, we recommend follow-up at the traditional four to six weeks with at least appropriate counseling on symptoms of progression to all patients and extended follow-up around three months in male eyes, pseudophakic eyes, eyes with lattice/peripheral retinal degeneration and eyes with history of retinal break or detachments in the fellow eye,” the researchers advised.
Patel PR, Minkowski J, Dajani O, et al. Analysis of posterior vitreous detachment and development of complications using a large database of retina specialists. Ophthalmology. November 14, 2022. [Epub ahead of print]. |


