 |
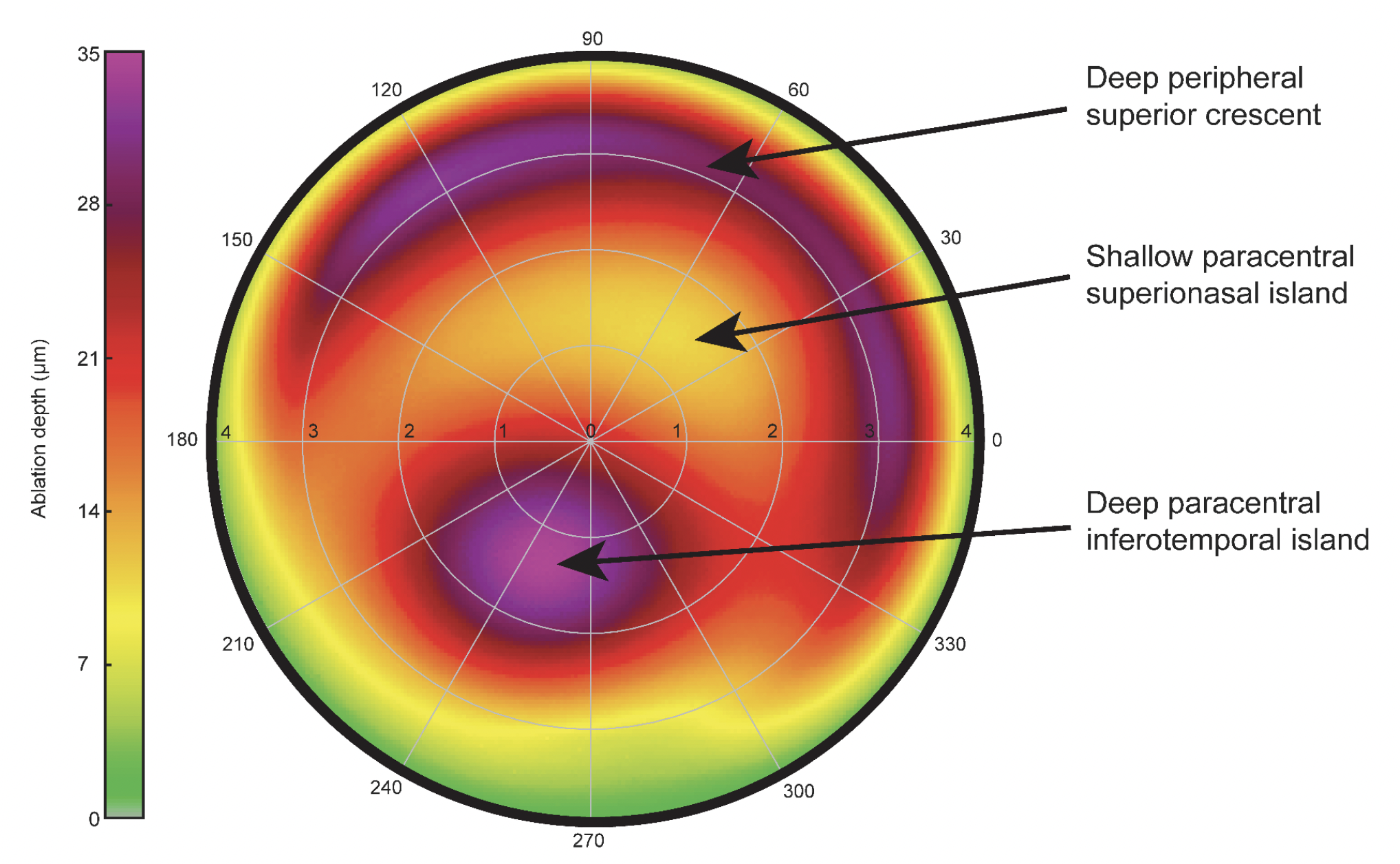
Like keratoconic eyes, postoperative ectasia often manifests with an inferiorly displaced cone, a unique and highly recognizable pattern on an HOA ablation map. Photo: Wallerstein et al. BMC Ophthalmol. 2023;23:517. Click image to enlarge. |
LASIK is safe and successful in nearly all patients, but there’s still concern about the risk of postoperative ectasia development, especially in individuals with thin corneas for which the residual stromal bed may fall below the standard cutoff of about 300µm. Doctors with access to a wavefront aberrometer may be able to pick up this surgical complication sooner, a new study suggests. Researchers sought to characterize anterior corneal higher-order aberration (HOA) excimer ablation map patterns in postoperative LASIK ectasia. As well, the researchers looked at correlations between newly identified HOA features in post-LASIK ectasia and known topographic indices.
Included in the prospective investigation were 28 total eyes of 22 post-LASIK ectasia patients. All HOA maps exhibited an arrangement of two elliptical paracentral ablation islands in direct mirror-like opposition to each other, one deep inferior and the other shallow superior. The deeper, inferior island was in the inferior quadrant in 100% of eyes and temporally in 92.3.% of eyes, while the shallow, superior island occupied the superior quadrant in 100% of eyes and nasally in 68.0% of eyes.
The deep inferior paracentral island ‘hot spot’ corresponded with the topographical apical POE cone and was highly reproducible in angular position. Ablation depth varied, and similarly, the superior crescents also displayed high depth variability. Both paracentral ablation islands stayed within a 3.4mm diameter central ring. The corneal irregularity index and ablation depth difference between deep and shallow paracentral islands exhibited a strong correlation with one another.
The authors contextualize these findings by stating that “while the use of wavefront aberration metrics is not new, the novelty of our work lies in the characterization of the HOA ablation map and its potential value as a diagnostic and monitoring tool for post-op ectasia,” the authors wrote in their paper on the study. Identifying the highly recognizable patterns in clinical practice—seen here in all 28 eyes—should lead to further investigation and OCT epithelial imaging to confirm the diagnosis, they added.
Elaborating on this research, the researchers suggest that these maps are particularly useful because they provide additional information related to position, eccentricity, depth, orientation and shape of anterior corneal HOAs, unlike Zernike whole-eye HOA values. This is the first study to have analyzed HOA ablation maps for ectasia eyes and objectively quantify the geographical representation of anterior corneal HOAs, deriving from them seven objective descriptors from four ablation islands.
These findings may also be able to quantify post-LASIK ectasia severity. The amount of coma reflected by corneal irregularity increased as the difference between ablation depth of both deep and shallow ablation islands increased. Consequently, the difference of depth between the two islands may be able to serve as a novel metric when quantifying the severity of cases.
Overall, the authors are hopeful that “the corneal HOA ablation map can potentially yield new information that can be used to diagnose, grade and monitor” post-LASIK ectasia progression both before and after corneal crosslinking, they concluded.
Wallerstein A, Santhakumaran S, Tabunar L, Cohen M, Gauvin M. Characterization of postoperative LASIK ectasia features on higher-order aberration excimer ablation maps. BMC Ophthalmol. 2023;23:517. |

