 |
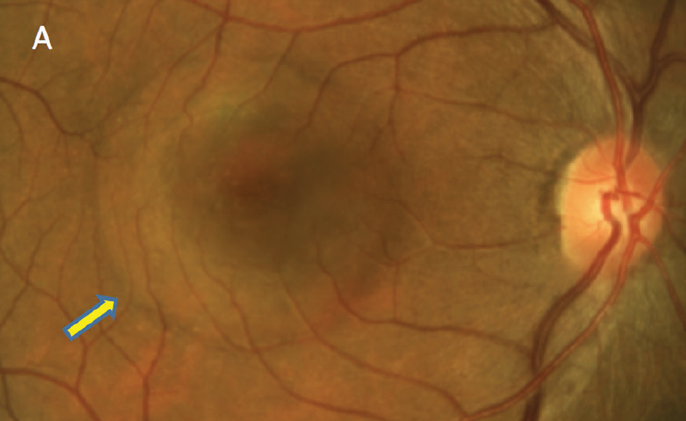
| The reduction in parafoveal GCC and foveal outer nuclear layer thicknesses in patients with central serous chorioretinopathy, in the absence of subretinal fluid, was found with OCT. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Central serous chorioretinopathy is usually associated with alterations of the retinal pigment epithelium and choroidal disturbances that may eventually result in the collection of subretinal fluid. This disease typically affects middle-aged males who may complain of blurred vision and metamorphopsia. Researchers recently evaluated OCT in the identification of clinical and structural features associated with metamorphopsia in patients with resolved chronic central serous chorioretinopathy. They found that clinical aspects (e.g., number of previous recurrences) and structural changes such as thinning of the ganglion cell complex (GCC) and optic nerve layer are common in individuals with metamorphopsia after subretinal fluid resolution.
The study, published in Retina, retrospectively analyzed 100 participants with resolved (absence of subretinal fluid) chronic central serous chorioretinopathy. Patients underwent a complete ophthalmological evaluation including assessment of metamorphopsia. The researchers noted that 66% of patients complained of metamorphopsia.
Compared with patients without distorted vision, both the foveal and parafoveal GCC thicknesses were thinner in central serous chorioretinopathy eyes with it (35.1μm and 82.0μm vs. 40.7μm and 93.1μm). In the foveal region, the outer plexiform layer and outer nuclear layer thicknesses were thinner in patients with metamorphopsia (24.6μm and 63.1μm vs. 29.1µm and 76.2μm). The ellipsoid zone band was more frequently discontinued in metamorphopsic eyes (56.1 % vs. 35.3%).
Regression analysis demonstrated that the strongest associations with metamorphopsia were parafoveal GCC thickness, foveal outer nuclear layer thickness and number of previous recurrences of subretinal fluid accumulation. The time interval from the last subretinal fluid resolution was not associated with the presence of visual distortion. The researchers noted that this last finding “suggests that this symptom does not disappear quickly and may eventually last months or be permanent.”
“The absence of a correlation between these two variables in individuals with central serous chorioretinopathy but without metamorphopsia (i.e., except in the perifoveal region) suggests the presence of a pathological dysregulation in presence of this visual phenomenon,” the researchers wrote in their paper. “We can speculate that a damage of photoreceptors in these eyes may result in a post-receptoral loss as explanation for the observed inner retinal thinning.”
The team concluded that structural parameters may be useful for clinical assessment of these patients and that their findings may be employed to guide the optimal anatomic target in individuals with central serous chorioretinopathy.
Borrelli E, Barresi C, Battista M, et al. Prevalence and morphologic biomarkers of metamorphopsia in eyes with “resolved” chronic central serous chorioretinopathy. Retina. May 23, 2023. [Epub ahead of print]. |


