 |
|
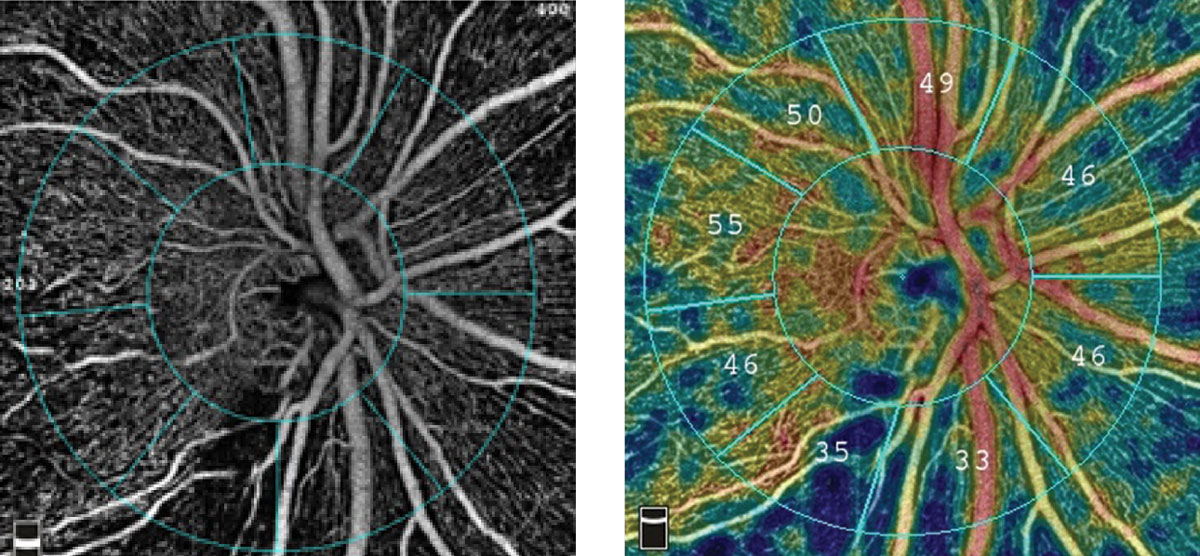
The radial peripapillary capillary angiogram, at left, and vessel density map, at right, show an inferior temporal wedge defect with reduced vessel density in a patient with primary open-angle glaucoma. Photo: Optovue. Click image to enlarge. |
The vascular underpinnings of glaucomatous damage continue to be revealed as OCT angiography becomes a more mainstream tool, and certainly a staple of research. A recent analysis of glaucoma patients with myopia explored the connection between visual acuity and various structural factors. Based on their findings, the study authors were able to link decreased visual acuity to specific locations suffering damage as well as the status of blood flow in the optic nerve head.
This retrospective cross-sectional study included 65 eyes of 60 myopic glaucoma patients without media opacity and retinal lesions. The study authors performed SITA 24-2 and 10-2 visual field testing.
OCT-A was used to evaluate superficial and deep vessel density in the peripapillary and macular regions. Retinal nerve fiber layer (RNFL) and ganglion cell-inner plexiform layer (GCIPL) thicknesses were also measured. Researchers defined decreased visual acuity as best-corrected VA <20/25.
Data showed that the presence of central visual field damage in glaucoma patients with myopia was associated with the worse mean deviation of SITA 24-2 as well as thinner GCIPL thickness and lower deep peripapillary vessel density.
Additionally, logistic regression analysis showed a correlation between decreased visual acuity and the following factors: thinner GCIPL thickness, lower deep peripapillary vessel density and longer disc-fovea distance.
The study authors reported that lower visual acuity was associated with thinner GCIPL thickness, lower deep peripapillary vessel density and larger β-zone peripapillary atrophy (PPA) area. They also observed a positive correlation between deep peripapillary vessel density and GCIPL thickness; however, no relationship was found between deep peripapillary vessel density and RNFL thickness.
“Decreased visual acuity in addition to central visual field damage was found in glaucoma eyes with myopia with low deep peripapillary vessel density and papillomacular bundle defect,” the study authors noted in their paper published in American Journal of Ophthalmology. “Additionally, structural parameters, such as long disc-fovea distance and large β-zone PPA were associated with visual acuity loss in glaucoma patients with myopia.
“Decreased deep peripapillary vessel density and papillomacular bundle defects may result from peripapillary sclera deformation by myopia, and this could be related to early visual acuity loss in these patients,” they concluded. They recommend the use of OCT-A imaging to monitor choriocapillaris within the peripapillary sclera which could assist in the prediction of VA among this patient population.
Kim SA, Park CK, Park HYL. Factors affecting visual acuity and central visual function in glaucoma patients with myopia. Am J Ophthalmol. May 11, 2023. [Epub ahead of print]. |


