 |
|
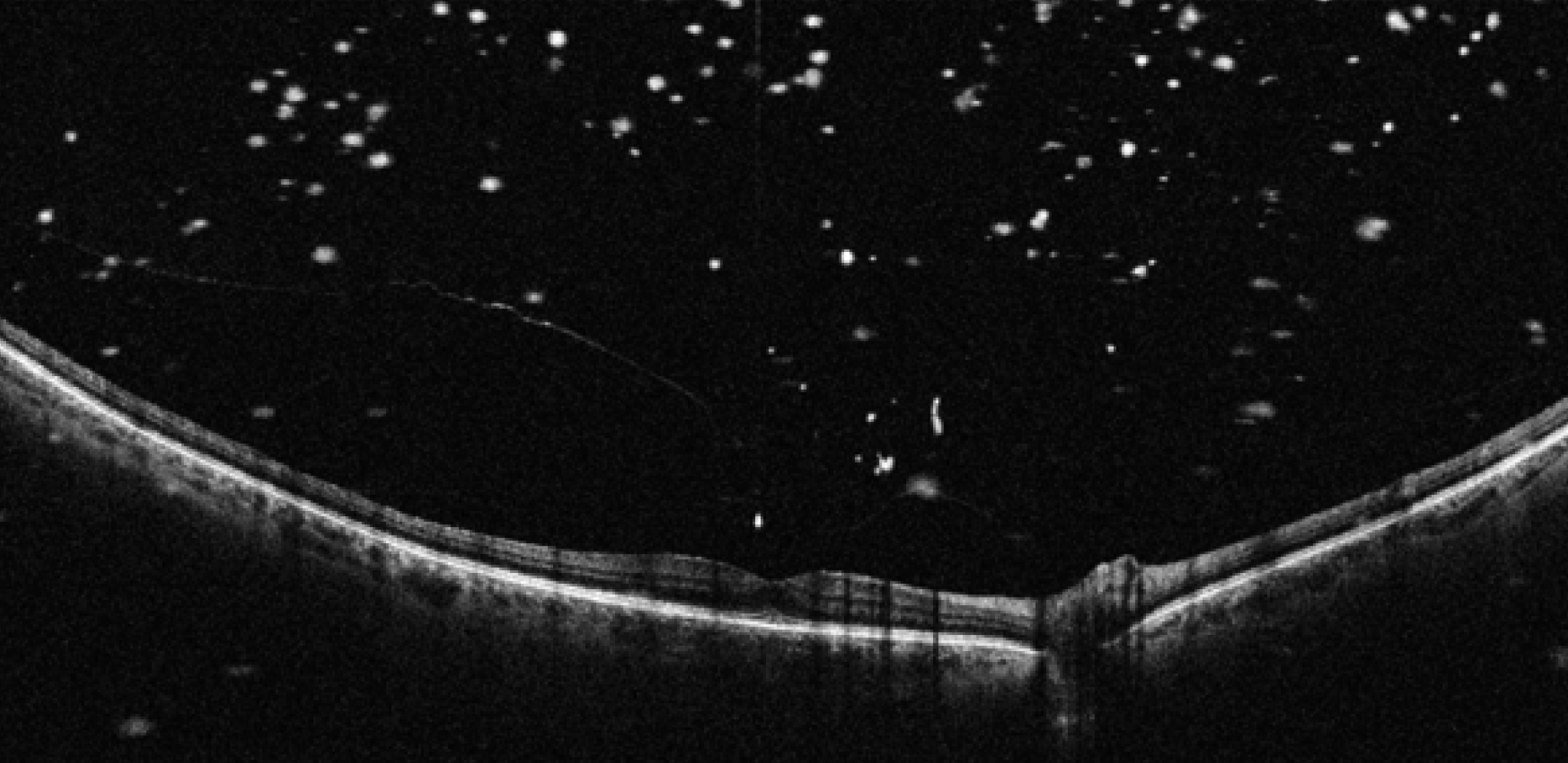
Posterior vitreous opacity and vitreomacular traction in a patient with with subfoveal outer lamellar macular hole and initial foveal schisis. Photo: Ripa M, et al. Diagnostics 2022, 12, 2247. Click image to enlarge. |
New research appearing in Retina aims to give guidance on how to better anticipate risk of retinal break following posterior vitreous detachment (PVD). With 388 patients, this is the largest study conducted concerning the association of posterior vitreous opacity (PVO) with in these patients, the authors note in their article on the work.
The study followed a retrospective design and collected the medical records of the patients. Included were those who previously received a PVD diagnosis and presented with flashes and/or floaters. Their OCTs were then reviewed for PVO presence, and the primary outcome found upon review was retinal tear presence on the fundus.
Of the 23.2% of patients found to have a retinal tear or dilated fundus, 86.7% of these displayed vitreous opacity presence on OCT as well. Upon this finding, a significant relationship was determined to exist between vitreous opacity presence and retinal tears.
Under these conditions, prompt diagnosis and treatment are vital to avoid vision threatening complications from occurring, like retinal detachment. The researchers mention potential risk factors to be aware of, such that previous studies found more frequent and faster progressing PVD in females. This was not consistent with the study’s findings, though, as they found males at higher risk of retinal tear. This was hypothesized to be resultant of morphological differences of the vitreoretinal surface.
When looking at symptoms telling of risk, the researchers found that isolated floaters predicted retinal tears in acute PVD patients. Instances of floaters and flashes or isolated flashes both were found to conversely be somewhat protective against retinal tears. This finding was in line with previous studies citing similar results.
As well as elucidating a connection between retinal tears and vitreous opacities, the study corroborated finding the most well-known risk factors associated with tears, including Shafer’s sign, vitreous and retinal hemorrhages. The team found the diagnostic specificity of each to be as follows: presence of floaters (63.4%), presence of Shafer’s sign (96.6%), presence of vitreous hemorrhage (88.9%) and presence of PVO by OCT imaging (72.5%).
The reason for the connection, the researchers posit, is that “opacities likely represent RPE cells liberated from the tear or red blood cells from vitreous hemorrhage.” Backing this up are their results that Shafer’s sign and vitreous hemorrhage were significantly associated with vitreous opacity upon OCT.
Based on the findings, the authors of the study suggest that “given the high risk of progression from retinal tear to detachment, it is imperative to rule out retinal breaks in patients with an acute PVD. Therefore, clinicians should have a low threshold to obtain an OCT in acute, symptomatic PVD cases.” Since the findings displayed high sensitivity (high instance of correctly identifying the disease), the authors add that absence of vitreous opacities may confirm a negative physical examination.
Rao AV, Shah AR, Nguyen VT, et al. Use of optical coherence tomography in detecting retinal tears in acute, symptomatic posterior vitreous detachment. Retina. 2022. [Epub ahead of print]. |


