At the AAO meeting’s first Academy Classroom Exchange (ACE) course, “Prescribing Prism for Binocular Disorders,” attendees were able to learn from Kelly Frantz, OD, and ask her questions in real time about their thoughts on the five cases she presented and how to better understand the approaches discussed. The innovative session took place this morning to kick off Day 3 of the Academy 2020 At Home educational program.
Many patients with binocular vision disorders have significant ocular discomfort, headaches and sometimes double vision when reading and using computers. With her examples, Dr. Frantz provided valuable methods of determining an appropriate prism prescription for certain characteristics to help relief patient symptoms.
Prism in Practice
Dr. Frantz began with discussing the advantages and disadvantages of using relieving prism, or neutralizing prims of the angle of deviation. “The big point for relieving prism for a patient with a binocular problem is that we would reduce the amount of vergence demand of that patient has to deal with," she said.
 |
| Figure 1. Dr. Frantz used the Bernell Test Lantern with the fixation disparity slide to determine the associated phoria. |
Since prism cannot address every condition a patient might present with, Dr. Frantz made many suggestions such as treating oculomotor disorders and vergence facility problems with vision therapy to develop faster skills with the patients' fusion vergence system as well as vision therapy and sometimes lenses for accommodative problems. “But prism can help individuals who have a large phoria and inadequate vergence ability to handle that deviation,” she noted.
The discussion then focused on the possibility of prism adaptation, or when the angle of deviation increases by up to the full amount of the prism. “Rather then just allowing the prism to help them fuse, the patient has actually made a divergence movement in response to the base-in prism, and their angle has gotten larger,” Dr. Frantz said. “If that were to happen, you've not done anything irreparable to that patient, they're just not a good candidate for prism.”
She noted that some people might not adapt fully that quickly to prism when wearing trial lenses in-office for 10 or 15 minutes, so she suggested can put a press-on Fresnel prism on their glasses for a week or two to determine whether the patient is comfortable and have them back in the office to see if they've adapted.
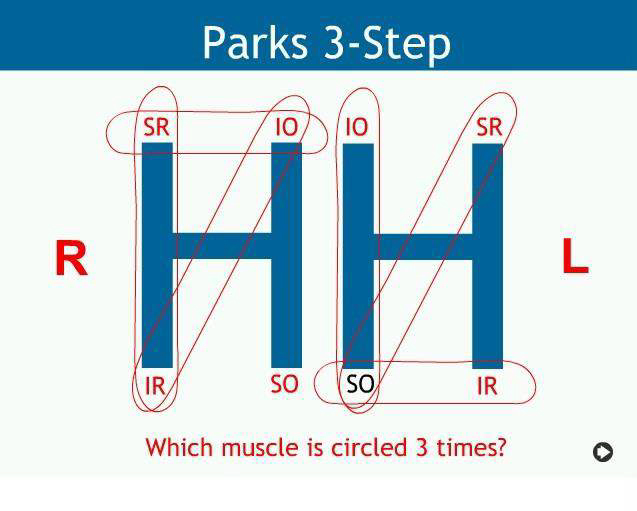 |
| Figure 2. In this Parks 3-step test, the left superior oblique was determined to be the underacting muscle in this noncomitant deviation patient. |
Dr. Frantz indicated that those with a normal visual system and good sensory and motor fusion are usually not the individuals that can be helped with prism.
“However, the people we can help most with prism prescriptions are those with normal sensory ability, good stereopsis and blend the two images together but they don't have the vergence ability to do the motor aspect very well,” Dr. Frantz said.
When assessing a patient with divergence insufficiency (DI), Dr. Frantz discussed assessing the distance-associated phoria, or the prism needed to neutralize the fixation disparity, to zero. She defined this fixation disparity as the small misalignment that can present in some patients even while they're fusing.
She also noted practitioners should also rule out pathological causes in the event of recent onset with neurological symptoms. Dr. Frantz also talked through Saladin's 1:1 rule for basic esophoria, which is to prescribe base-out prism to make esophoria equal to their base-in vergence recovery. “It works pretty well for eso at distance,” she noted.
A Role for VT?
In a patient with convergence insufficiency, Dr. Frantz mentioned an initial treatment of vision therapy. She noted to only consider prism for near unless the patient can tolerate full-time wear. Dr. Frantz reminded everyone that Sheard's criterion says that the base out to blur needs to be twice the phoria. She recommended this method to prescribe prism for exophoria of 4∆ or greater at far and near.
Equations for Esophoria and ExophoriaHere are some equations that Dr. Frantz highlighted when dealing with esophoria and exophoria. Saladin’s 1:1 Rule for Esophoria Example: Patient has 8∆ esophoria with BI range x/4/2 BO ∆= (phoria - BI recovery)/2 = (8-2)/2 = 3∆ BO Prescribe 3∆ BO for equal esophoria and BI recovery
Sheard’s Criterion for Exophoria BI ∆= [2(exophoria) - BO range to blur] Example: Near phoria: 16∆ exo; near BO vergence: x/24/16 Sheard’s ∆= [2(16)-24]/3 = 2.67∆ Trial framed 3∆ BI; patient preferred this to no prism |
When an attendee asked a question regarding convincing parents that their children need vision therapy, Dr. Frantz emphasized not to promise that base-in prism alone could take care of the whole problem. “The system's more complex in children because they have all the interactions with accommodation and vergence,” she noted. “In a presbyopia individual, it's pretty much a vergence system with therapy.”
Dr. Frantz talked about how when a patient presented with vertical diplopia that was relieved with a head turn, that it can make you think of a noncomitant situation, possibly muscle paresis. She used the Parks 3-step test and circling technique as well as the Maddox rod test to determine the muscle paresis. If some fusion is possible in an extraocular muscle paresis, Dr. Frantz recommends using associated phoria, and if the patient has diplopia, she suggests determining the least prism to neutralize the diplopia subjectively. “If a patient has diplopia, then put up a discrete target for them to look at and add then prism of the appropriate base to neutralize the diplopia,” she said.
Before wishing her attendees luck with their patients, Dr. Frantz commented, “I hope what you learned today takes care the needs of your patients and getting more comfortable and able to look at screens for hours and hours lately, as so many of us are doing.”
