 |
|
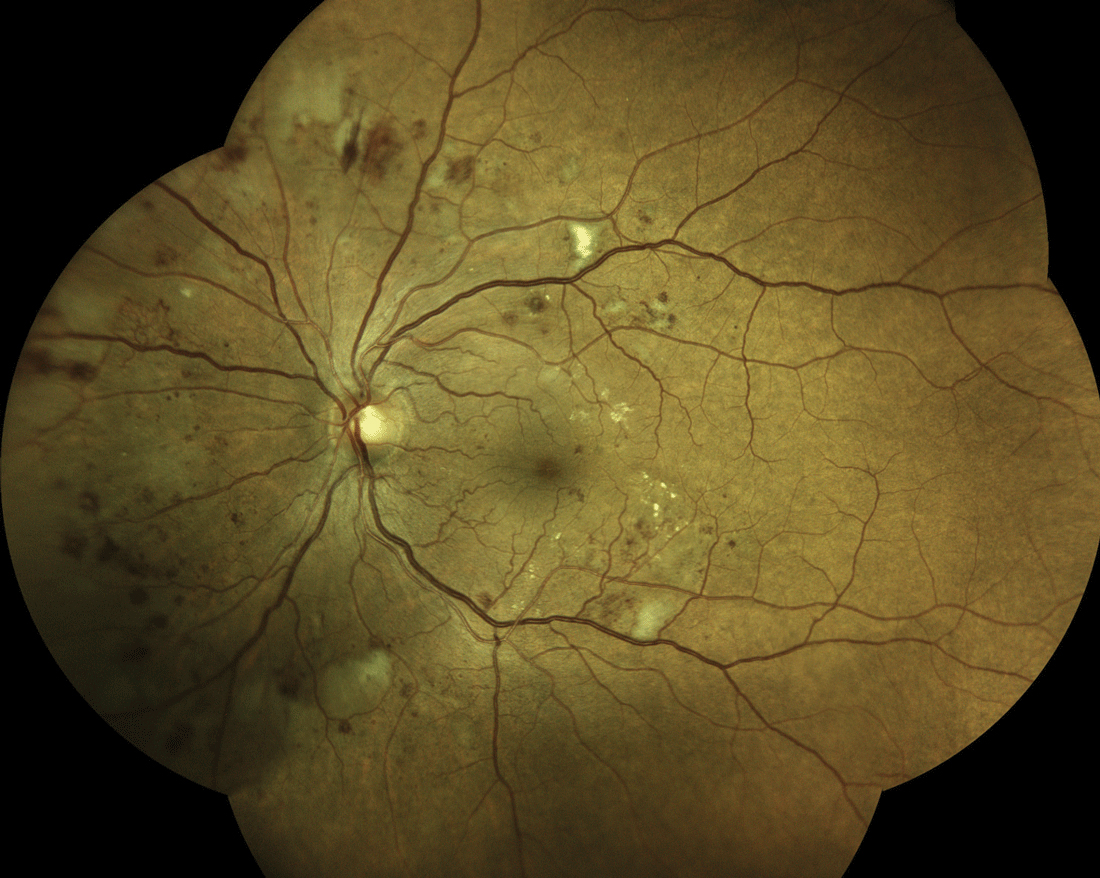
Using an AI system to screen patients with diabetes may have a time-saving advantage over human-based grading. Photo: Steven Ferrucci, OD. |
Artificial intelligence (AI) systems using digital fundus photography have been developed for diabetic retinopathy (DR) to address the increased demand for screening related to a burgeoning diabetic population. A study in Ophthalmology Science evaluated and compared the performance of an AI system and dilated ophthalmoscopy against the Early Treatment Diabetic Retinopathy Study (ETDRS) reference standard on the same large, diverse cohort of subjects enrolled at multiple centers with geographic diversity. It also reported and compared the performance of dilated ophthalmoscopy by general ophthalmologists and retinal specialists. The researchers found that the AI system had higher sensitivity for detecting more-than-mild DR than general ophthalmologists and retinal specialists as compared with the clinical reference standard. They believe it could potentially serve as a low-cost point-of-care DR detection tool and help address the diabetic eye screening burden, given the low compliance rate for annual diabetic retinal exams.
In 521 patients (999 eyes) who were 18 or older, had diabetes mellitus and underwent dilated ophthalmoscopy, 406 were examined by general ophthalmologists and 115 by retinal specialists. The reading center grading of four widefield stereoscopic dilated fundus photographs using the ETDRS severity scale reported 207 positive and 792 negative eyes for more-than-mild DR. Of these 999 eyes, 26 eyes were ungradable by the AI screening system.
Retinal specialists had 59.5% sensitivity and 98.9% specificity for more-than-mild DR vs. the AI system which had 97% sensitivity and 88% specificity. In a separate comparison, general ophthalmologists had 20.6% sensitivity and 99.8% specificity for more-than-mild DR, while the AI system had a 96.5% sensitivity and 86% specificity. Similar to the retinal specialists, the AI system did not miss any cases of vision-threatening DR, in contrast to the general ophthalmologist group.
The researchers noted that the significant discrepancy between the clinical reference standard grading and the retinal specialists is mainly due to undergrading of moderate nonproliferative DR as mild nonproliferative DR.
“An AI screening-based system is ideally one that has a high sensitivity in order not to miss significant pathology that could cause visual loss,” the researchers wrote in their paper. “Conversely, an ideal AI screening system would have a lower specificity in the trade-off between sensitivity and specificity when screening for potentially visual-threatening pathology.”
Disadvantages of the AI system include the somewhat lower specificity which may lead to over-referral. A significant portion of patients with false positives had mild nonproliferative DR or other ocular pathology that would benefit from evaluation by an ophthalmologist.
“Thus, use of the system should be tempered with the advice to seek a general ophthalmic examination if the patient has blurred vision or if the patient is in a high-risk group for conditions such as glaucoma,” the researchers noted.
Unlike human-based telescreening systems, they believe that an AI system provides an immediate determination of the presence of more-than-mild DR that is available to the patient prior to leaving the primary care office, which could improve adherence to follow-up care.
Lim JI, Regillo CD, Sadda SVR, et al.. Artificial intelligence detection of diabetic retinopathy: subgroup comparison of the EyeArt System with ophthalmologists' dilated exams. Ophthalmol Sci. September 29, 2022. [Epub ahead of print]. |


