 |
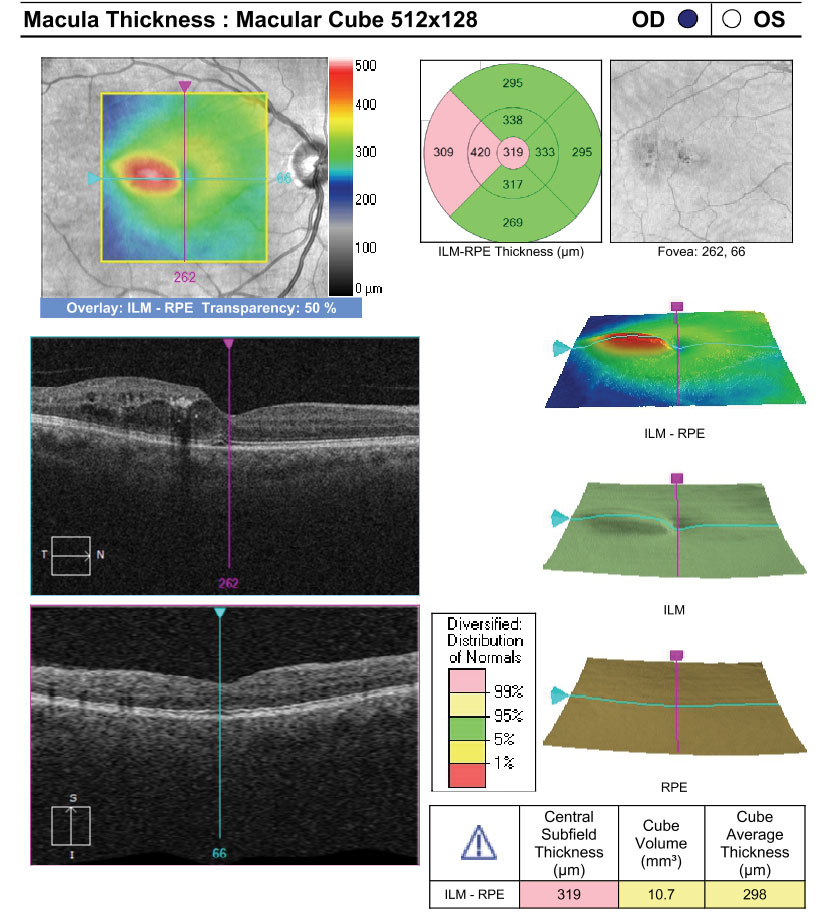
| Concerns about cataract development discourage steroid use in phakic DME patients, but this study found it might be advisable to shift from an anti-VEGF to anti-inflammatory agent if initial results prove suboptimal. Photo: Anna Bedwell, OD. Click image to enlarge. |
New research confirmed real-world data regarding the response to anti-VEGF treatment in diabetic macular edema patients with phakic eyes as well as the importance of baseline visual acuity and frequency of injections in predicting patient outcomes.
These recently published findings also demonstrated that continuing treatment beyond six months for suboptimal responders results in unnecessary treatment burden without a significant change in visual acuity.
This retrospective cohort study, which aimed to better understand the response to anti-VEGF treatment as well as shed light on associated treatment burden in this patient population, used electronic patient record data from 500 eyes of 399 patients at two UK centers between 2015 and 2020.
The study authors reported that anti-VEGF treatment for DME patients with phakic eyes in real-world UK clinical practice can maintain or improve vision. While the outcomes they found are worse than clinical trials, the team noted that this is consistent with real-world data. At six months, the results showed that 65.8% of phakic eyes had a suboptimal response to anti-VEGF treatment.
Baseline visual acuity was predictive of visual acuity outcome, according to the study authors, who reported that, despite greater gains in eyes with poorer visual acuity, these eyes did not achieve the same visual acuity levels as those who began treatment with better visual acuity.
In this analysis, 53.6% of eyes had more than three injections in the first six months. This suggests difficulties in the delivery of high volume/high frequency treatment, the researchers reported. Beyond six months, the data showed that optimal and suboptimal responders had similar ongoing treatment and review burden over four years of anti-VEGF treatment.
“It is recognized that clinicians would have adjusted their decision about retreatment and/or treatment intervals based on the absence of an increase in macular oedema,” the study authors concluded in their paper for the journal Eye. “Thus, for the suboptimal responders this treatment helped to maintain some visual acuity, but consideration should be given to early switch to longer acting treatments to reduce treatment burden and improve outcomes.”
Rennie C, Lotery A, Payne J, et al. Suboptimal outcomes and treatment burden of anti-vascular endothelial growth factor treatment for diabetic macular oedema in phakic patients. Eye (Lond). August 4, 2023 [Epub ahead of print]. |

