 |
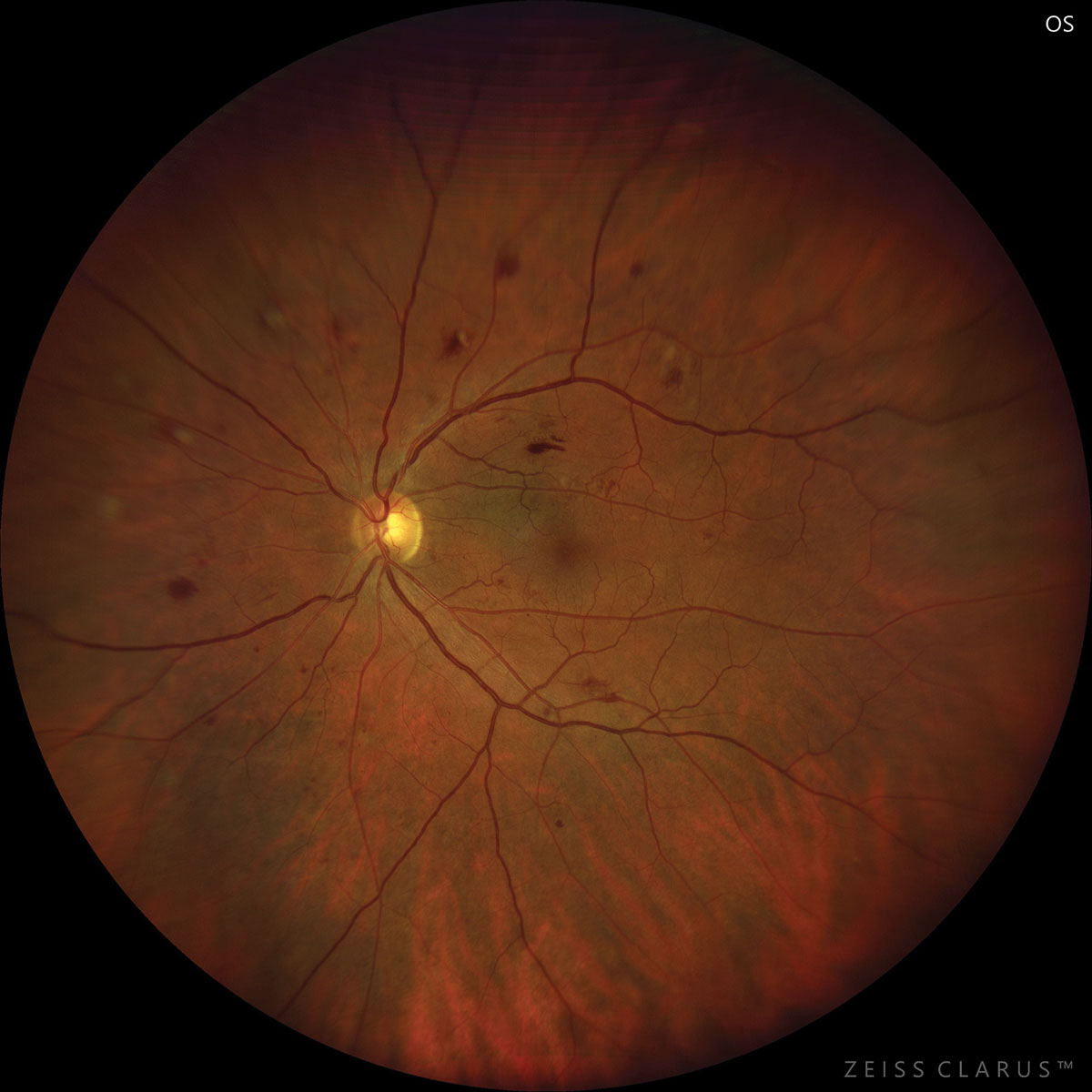
| Underuse of eye care in patients with greater social burdens was equal in its effects for type 1 and type 2 diabetes patients. Photo: Jay Haynie, OD. Click image to enlarge. |
Researchers recently wanted to evaluate the association of social determinants of health (SDoH) with ocular checkups or interventions. The retrospective study looked at 20,807 adults with self-reported diabetes using the 2013-2017 National Health Interview Study.
The SDoH included six domains: (1) economic stability, (2) neighborhood, physical environment and social cohesion, (3) community and social context, (4) food environment, (5) education and (6) healthcare system. An aggregate SDoH score was determined and divided into four quartiles, with Q4 distinguishing the highest adverse burden.
The researchers found that 43% of all participants had not pursued eye care within the last 12 months. A greater SDoH burden was associated with reduced likelihood of eyecare use, and this was the case across race and ethnicity. Those in the fourth quartile had a 59% lower chance of using eye care than those in the first quartile. Of all domains, the strongest association with eyecare use was economic stability.
“One’s family income and employment status certainly impacts quality of housing and physical environment, type of neighborhood that one lives in, food security, use of health information technology and health coverage,” they wrote in their paper for Ophthalmology.
Adjacent to the issue of housing, food insecurity was, understandably, also a risk factor for poor management of diabetes and adverse health outcomes. This may be caused by people opting for affordable, energy-dense but nutritionally lacking foods that raise serum glucose or diverting their money from purchasing food altogether. Lower education was also linked to poor vision outcomes and difficulties.
Outside of environmental factors, psychological distress can also impact individuals, as it was associated with all-cause mortality, cardiovascular disease and cancer mortality among adults both with and without diabetes. Health insurance also played a large role in the likelihood of pursuing care, accounting for a major risk factor of vision outcomes and eyecare use.
All of the SDoH adverse determinants had been previously linked with underuse of health care in general or poor health outcomes. Poor housing conditions were linked to lower eyecare use from a sample in Washington DC. Medicaid beneficiaries with diabetes and worse glycemic control received less social support in another sample.
Going forward, the researchers believe that “addressing adverse SDoH and connecting patients to needed services could be a means by which to improve eyecare utilization among people with diabetes and prevent vision loss.”
Taccheri C, Jordan J, Tran D, et al. The impact of social determinants of health on eye care utilization in a national sample of people with diabetes. Ophthalmology. June 15, 2023. [Epub ahead of print]. |

