 |
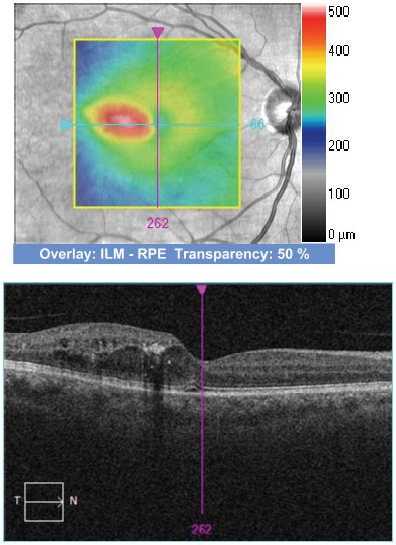
Calculating the proportion of time DME patients spend above different VA thresholds during anti-VEGF therapy may help evaluate visual outcomes over time. Photo: Anna Bedwell, OD. Click image to enlarge. |
Researchers recently put a new quantitative treatment response measure to the test in patients with diabetic macular edema (DME) receiving anti-VEGF injections. While clinicians often look at the mean change in visual acuity (VA) from baseline to tell whether a patient’s vision is improving, this measurement fails to determine the proportion of patients who achieve a clinically relevant threshold—i.e., VA required for driving—at various points throughout treatment. Observing patients’ best-corrected VA (BCVA) time in range could be a more effective way to describe visual outcomes and functions over time, the researchers suggest.
The study group performed a post-hoc analysis of the Protocol T randomized clinical trial, including 660 patients with center-involved DME and BCVA of 20/32 to 20/320. Patients received one of the following courses of treatment: intravitreal aflibercept 2mg, repackaged (compounded) bevacizumab 1.25mg or ranibizumab 0.3mg given up to every four weeks.
“Using a BCVA letter score threshold of ≥69 (20/40 or better), the least squares mean time in range (adjusted for baseline BCVA) in year one was 41.2 weeks with intravitreal aflibercept, four weeks longer than bevacizumab and 3.6 weeks longer than ranibizumab,” the researchers reported in their paper in Eye. They added that “mean time in range was numerically longer for intravitreal aflibercept for all BCVA letter score thresholds between 92 and 30 (20/20 to 20/250).”
Throughout year two, patients who received intravitreal aflibercept spent 3.9 weeks longer in range than those receiving bevacizumab and 2.4 weeks longer than those on ranibizumab.
“Between BCVA thresholds 20/250 to 20/15, patients receiving intravitreal aflibercept had consistently better time in range than patients receiving bevacizumab or ranibizumab,” the researchers pointed out in their paper. “Outside of this interval, where the sigmoid curve is horizontal, the time in range did not differentiate between the three anti-VEGF agents,” they added.
The researchers concluded that time in range may be a clinically relevant visual endpoint to assess functional outcomes over time in patients on anti-VEGF therapy for DME. They added that this metric could “provide a better understanding, for physicians and patients, of the consistency of treatment efficacy.”
Kozak I, Pearce I, Cheung CMG, et al. Visual acuity time in range: a novel concept to describe consistency in treatment response in diabetic macular oedema. Eye (Lond). March 28, 2023. [Epub ahead of print]. |

