 |
A 63-year-old Caucasian female whom I’ve been seeing for several years was recently referred for cataract surgery, as her cataracts had gradually progressed over the past several years and were beginning to affect her quality of life.
I first met this patient in 2018 when she was referred to me by her primary care provider with complaints of transient visual obscurations. At that time, she also complained of right-sided eye discomfort and transient visual obscurations OU lasting for a few minutes several times each day. The onset of symptoms had begun two weeks earlier, and when they did not subside, she sought the care of her primary care provider who referred her to me.
 |
The patient’s initial visit in 2018 showed only one isolated cotton wool spot along the inferior arcade, which is consistent with the iris neovascularization, ocular ischemia and complaints of visual disturbances. Click image to enlarge. |
Ultimately, the patient presented with neovascularization of the iris in the right eye and visual acuities of 20/25 OD and 20/20 OS. Medication included crestor, synthroid and albuterol PRN. Pupils were ERRLA with no afferent pupillary defect noted. The anterior segment was entirely normal otherwise OU, with clear crystalline lenses. Prior to dilation, threshold visual fields were performed and showed generalized depression OU; there were no neurological field defects respecting the horizontal or vertical meridians. Applanation tensions were 18mm Hg OD and 17mm Hg OS. Cup-to-disc ratios were 0.50 x 0.60 OD and 0.50 x 0.55 OS. There was no neovascularization of the disc nor elsewhere in either eye. There was one isolated cotton wool spot (microinfarct) along the inferior arcade in the right eye, and vasculature OU was characterized by mild arteriolarsclerosis. The peripheral retinal examination was unremarkable. Baseline multimodal fundus images were obtained.
Auscultation for carotid bruits was positive on both the right and left sides. Given the clinical findings, the patient was scheduled for a carotid Doppler evaluation followed by an MRI and MRA. The studies demonstrated >90% occlusion of the right internal carotid artery and >75% of the left. MRI findings demonstrated several areas of focal atrophy consistent with small vessel occlusive disease, and the MRA demonstrated stenosis of various branches of the cerebral vasculature, in particular the left posterior cerebral artery (PCA).
The patient was scheduled for a right carotid stenting procedure, which was completed without complication. During the carotid stenting, a cerebral angiogram was performed, which verified the stenosis of the left PCA. The patient was subsequently scheduled for stenting of the left PCA. She returned for this procedure; however, intraoperatively it was found that this vessel was not amenable to stenting, so the procedure was aborted.
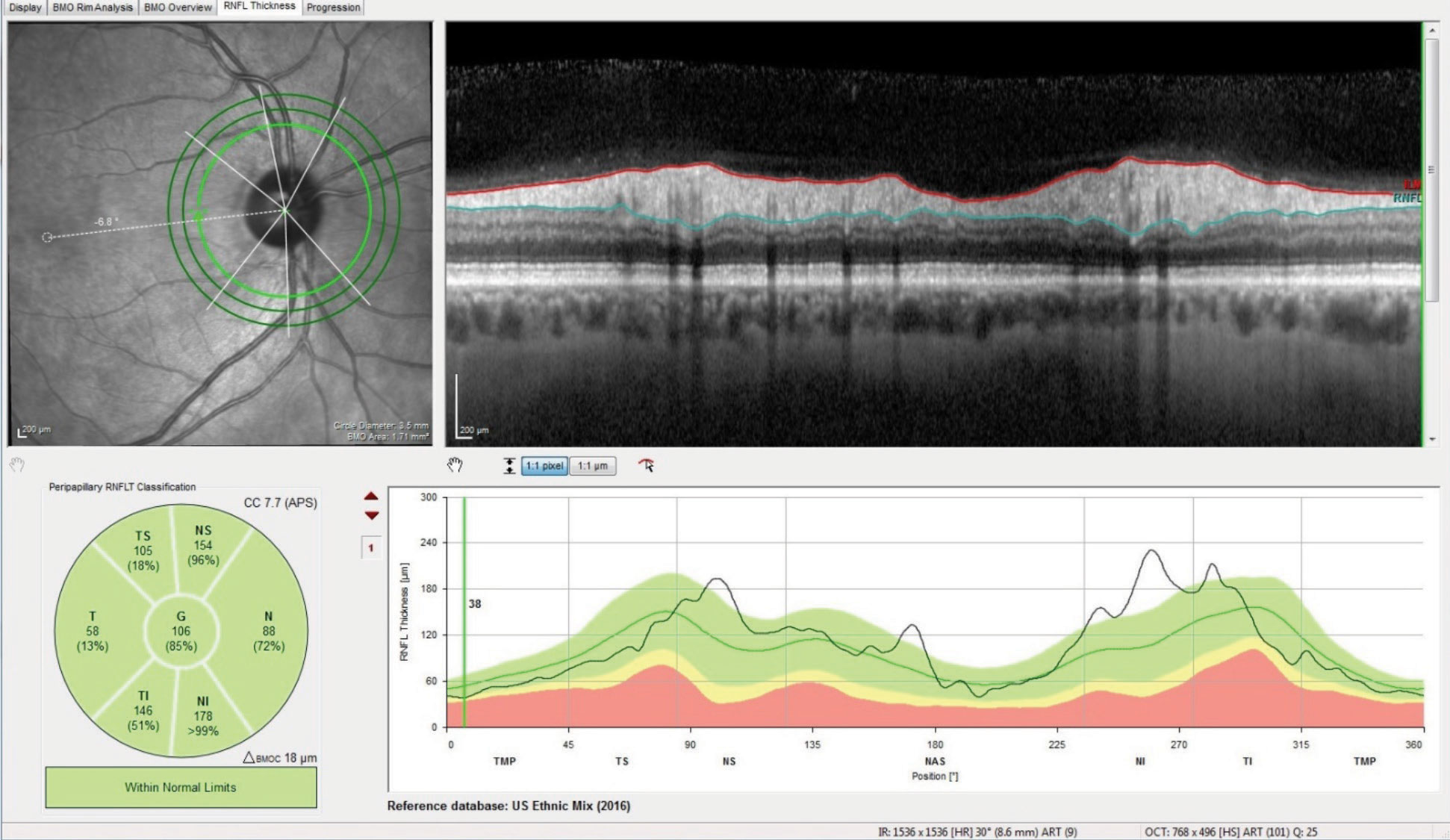 |
Baseline RNFL 3.5mm circle scans were obtained following the carotid artery stenting and failed PCA stenting. This image was taken three months after initial presentation. Click image to enlarge. |
Approximately three months following the carotid stenting, the patient’s neovascularization had cleared, as did the microinfarct seen funduscopically in the right eye on initial presentation. Also, she was free of symptoms related to visual obscurations. Baseline OCT scans were obtained.
Following two years of close surveillance of her ophthalmic and visual status and with no complications, the patient was scheduled to be seen yearly and was compliant with the visits. No other neurological symptoms developed in this timeframe, though she did begin to develop cataracts, and as time progressed, the cataracts began to affect her quality of life.
As is always the case in our office, a pre-cataract surgical evaluation was completed prior to referral to the cataract surgeon. This included a detailed and dilated fundus examination, OCT scans of the optic nerves and maculae, tonometry, A-scan ultrasonography and IOL calculations. There were no noted contraindications to cataract surgery, and a preliminary appointment was made with the cataract surgeon. Medications at this point in early March included the previous listed medications along with dabigatran, olmesartan and carvedilol.
Following the evaluation of the patient by the cataract surgeon, she was referred back to me for evaluation of glaucoma OD prior to scheduling lens extraction with IOL placement. Of note was the cataract surgeon’s concern that there was RNFL thinning on the right eye consistent with glaucomatous damage.
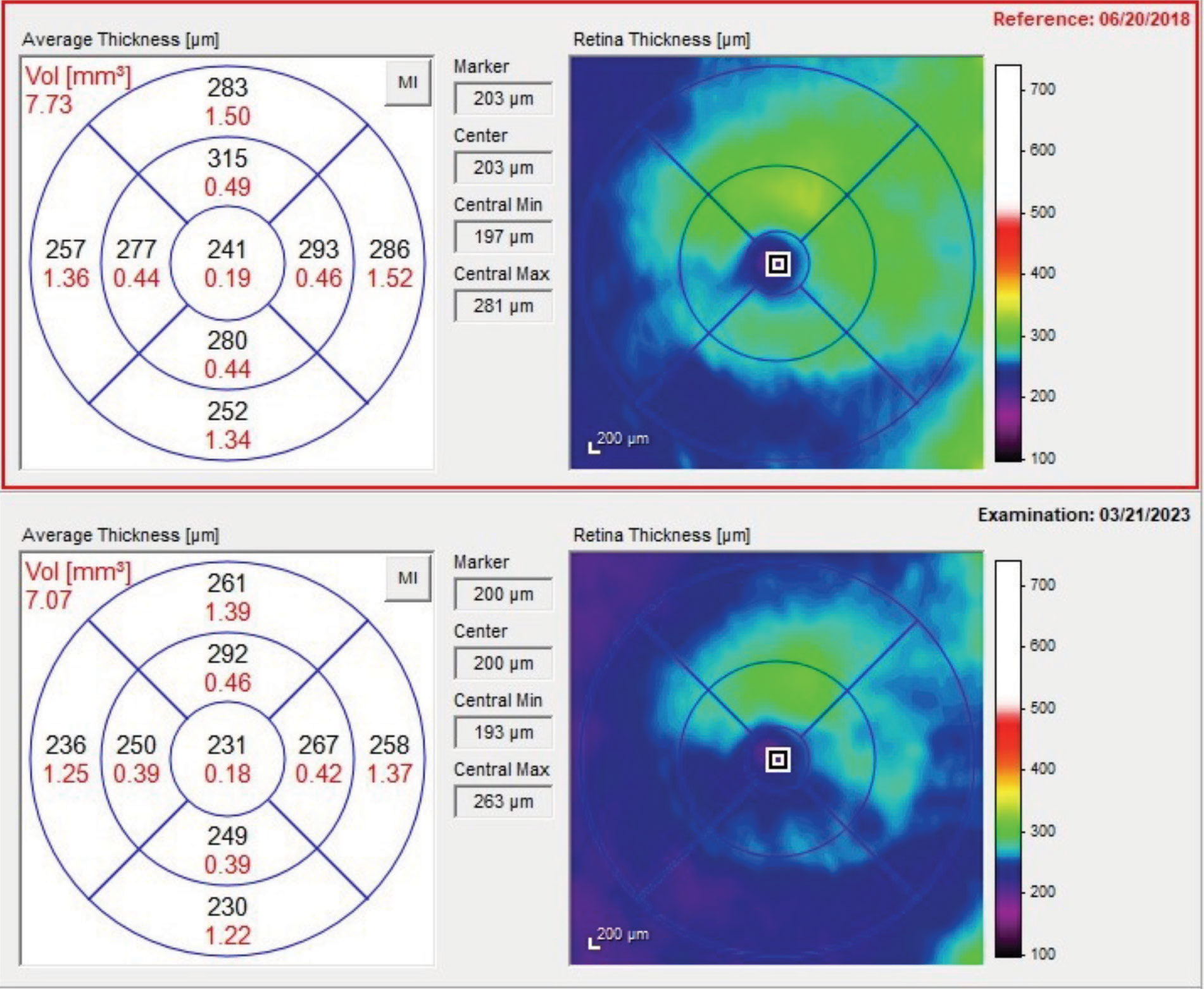 |
Retinal thickness changes seen from the baseline scan in 2018 to the most recent scan in 2023. Note the significant thinning of the retina in the inferior temporal arcuate region. Click image to enlarge. |
The patient returned to my office for evaluation. Intraocular pressures were found to be 18mm Hg OD and 19mm Hg OS. Her cup-to-disc ratios were unchanged from previous visits, and glaucoma OCT scans were obtained. There were no changes from scans of the past four years. Gonioscopy showed open angles with no neovascularization and minimal trabecular pigment OU. Threshold field studies were essentially unremarkable.
While there were no recent changes in her OCT scans, there were changes in her right eye that were attributable to the ocular ischemia she presented with in 2018. As the scans showed, there were changes in the macular thickness scans in the right eye that are sometimes suggestive of glaucoma.
Keep in mind that when viewing the macular scans, the cataract surgeon was only seeing the current scans, which do in fact show thinning of the inferior temporal arcuate region; this finding is what raised the alarm with the cataract surgeon that glaucoma may exist. Closer examination of her earlier scans also shows some early changes seen in the same scan in 2018. Remember too, that this 2018 scan was taken about three months following the carotid stenting on the same side, and the OCT from 2018 is consistent with early ischemic damage to the retina consistent with the ocular ischemia that was ongoing at that time.
The GCL shows similar changes. Note the relatively robust GCL thickness in the 2018 scan, relatively early in this disease process.
The neuroretinal rim in the right eye at the current time is stable, with no glaucomatous tissue loss. There is some subtle pallor in the temporal aspect of the rim, owing to the ischemic tissue loss secondary to the ocular ischemic syndrome that initiated sometime prior to our first visit in 2018.
And herein lies the lesson of this case: glaucomatous damage can certainly result in loss of the RNFL and GCL in the macula, but it also manifests in loss of neuroretinal rim tissue at the disc. Various OCTs measure the neuroretinal rim tissue in different ways, but looking closely at the minimum rim width adjacent to Bruch’s membrane opening is very helpful in noting erosion of neuroretinal rim tissue. This patient had none, indicating that these changes were associated with neuropathy that is not glaucomatous in origin.
There are other conditions that can cause loss of the ganglion cell and RNFL layers without neuroretinal rim loss, and they include the non-glaucomatous optic neuropathies, retinal artery occlusions and other vascular ischemic events, to name a few. In these cases, the loss of the RNFL and GCL occurs quickly, usually within six months of the event. Neuroretinal rim tissue is not lost, but it often becomes pallid.
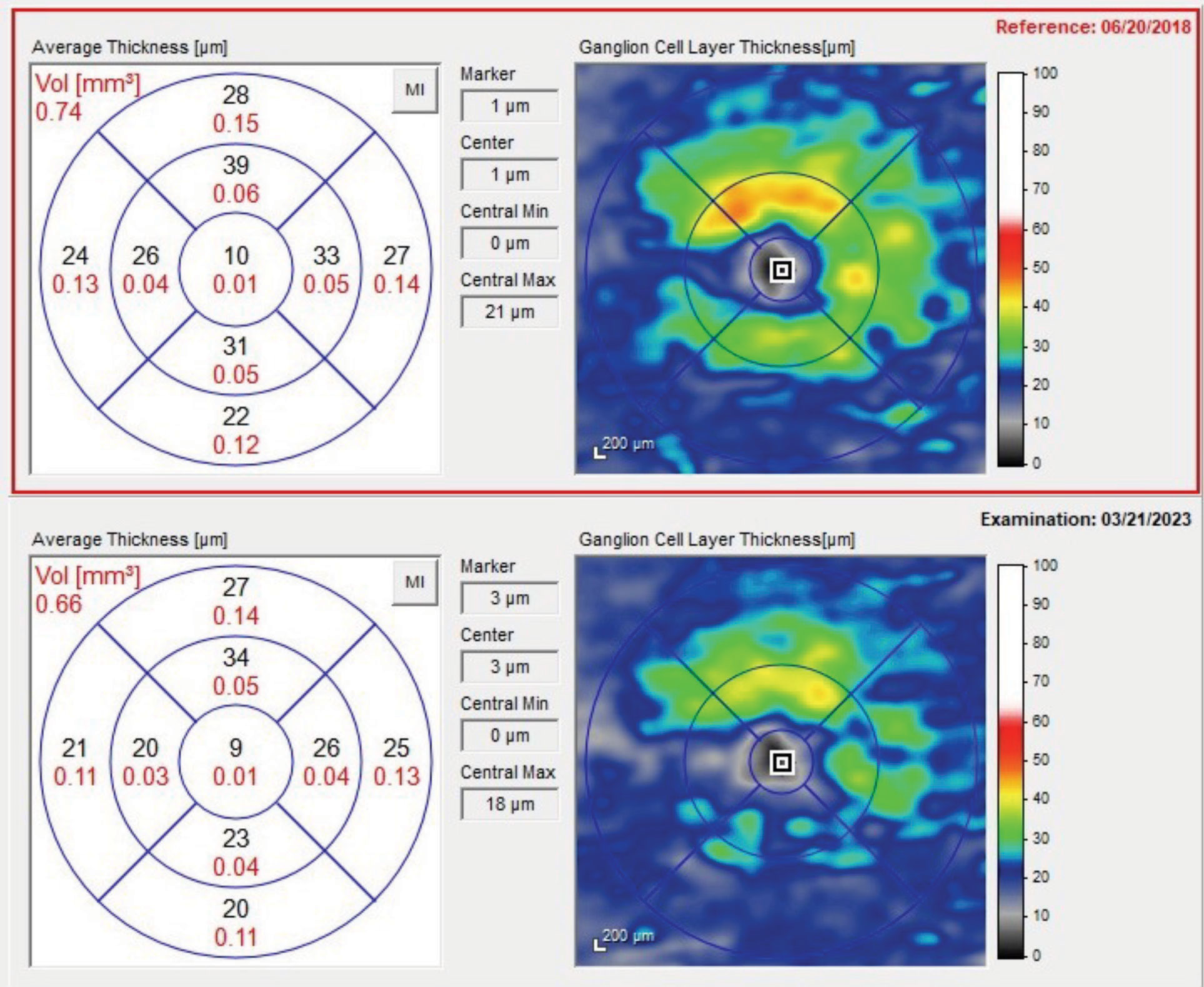 |
The baseline and current GCL thickness maps. Note the significant loss of thickness seen in the 2023 scan. Click image to enlarge. |
Outcome
While a quick look at a macular scan preoperatively raises the spectre of glaucoma, the back history of this patient tells us the whole story: what we are looking at today is damage that occurred five years ago due to perfusion issues, which have remained stable and since been rectified.
What kind of visual recovery should this patient expect following cataract surgery? Well, her best-corrected visual acuity two years ago (prior to significant cataract progression) was 20/25 OD and 20/20 OS. Snellen acuity post-lens extraction (barring any complications) will probably be good, perhaps 20/25 OU, but I would suspect that the patient will always see a difference between the eyes, with the left being subjectively better than the right. This was discussed with the patient again before she was referred back to the cataract surgeon for the lens extractions.
The damage has been done; now let’s get the patient seeing to her best ability while still surveilling for progressive atherosclerosis of the visual system.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

