 |
Q:
I have a patient interested in refractive surgery but they have borderline dry eye (decreased tear breakup time and some symptomatic complaints but no evidence of staining). What’s the best course of action? Would this be a patient more suited for SMILE rather than LASIK? Either way, what are some best practices for follow-up care?
“As a first step, it is highly recommended that dry eye should be treated using standard treatment, such as artificial tears and/or anti-inflammatory agents before any refractive surgery,” says Cecilia Chao, BOptom, PhD, of UNSW Sydney’s School of Optometry and Vision Science. She explains that improvement in dry eye signs and symptoms, such as dryness, grittiness or tearing, as well as their severity, should be recorded. This can be done with a validated questionnaire, like the Ocular Surface Disease Index, Ocular Pain Assessment Survey or Ocular Comfort Index. In addition, for mild dry eye, carefully review the patient’s systemic health, medication use, previous eye and other surgeries and even mental health, as all these components are needed to clear the potential risk factors that may be associated with development of post-LASIK neuropathic dry eye.
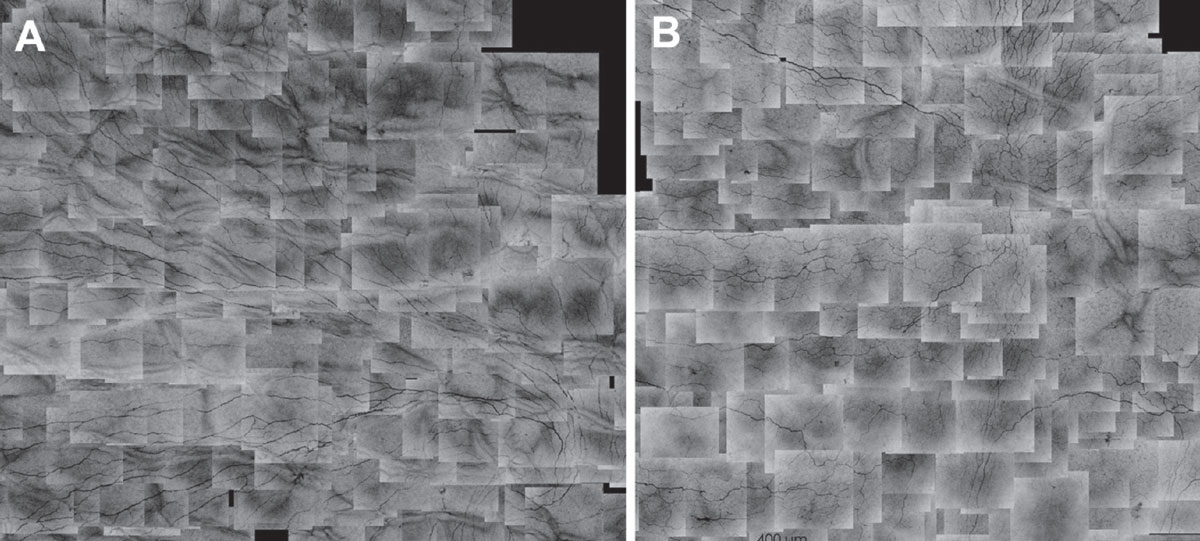
“If dry eye symptoms cannot be relieved with typical treatment and the patient may have normal tear function with minimal to no corneal/conjunctival staining, mild neuropathic pain should be considered. The persistent symptoms can be confirmed using the validated questionnaires,” Dr. Chao continues. If in vivo confocal microscopy (IVCM) is accessible in your clinic, it can further confirm the health of the corneal nerves and immune response through examination of corneal nerve integrity, the presence of corneal immune cells and morphology. It is the surgeon’s or optometrist’s responsibility to explain to patients the potential risk or further damage that can occur to the corneal nerves after surgery, as well as outline the potential to suffer from greater and persistent ocular neuropathic pain, she adds.
Surgery Effects
Regarding whether SMILE is superior to femtosecond-LASIK (FS-LASIK), there is still limited evidence. It’s been shown that there are fewer short-term incidents of postoperative dry eye after SMILE compared with LASIK, but long-term effect is still undetermined, Dr. Chao says. In addition, SMILE presents a more technical challenge due to the complexity of the procedure. This results in more intraoperative discomfort and greater visual symptoms after surgery when compared with LASIK. Therefore, it is all dependent on the expectation of the patient and the experience of the surgeons.
“Based on my experience, for follow-up after FS-LASIK, we use 0.5% levofloxacin four times a day for three days and 0.1% fluorometholone four times a day for one week,” Dr. Chao notes. “The fluorometholone is tapered weekly and stopped by week four post-op.”
It is vital not to drop the fluorometholone from four times a day to none for any type of refractive surgery, she warns. In addition, all refractive surgery patients should be instructed to use nonpreservative artificial tears at least four times a day and for at least six months, since corneal sensitivity will not return to normal anywhere from six to 12 months. Apart from a slit-lamp test, it is highly recommended to do sensitivity and IVCM testing every visit, along with monitoring the symptoms using a validated questionnaire, starting from one month after operation, she adds.
 |
|
Corneal subbasal nerve map of emmetropic right eye of a normal subject (A) and right eye of another subject seven years after LASIK (B). Shown at 400mm of the scale bar. Click image to enlarge. |
Dr. Chao highlights that usually, if patients suffer from neuropathic dry eye more than one year after the surgery, there may be minimal slit lamp and abnormal tear film function findings for an optometrist to observe. To combat this issue, hyperosmolar saline may be used as a diagnostic test before the surgery. “A more recent study in FS-LASIK outlines corneal dendritic cells (immune cells) and corneal nerves’ interaction,” Dr. Chao notes. “If IVCM is accessible, I would suggest looking at the cell morphology, since it is related to the ocular immune response.” She also explains that there may be more migratory cells after LASIK, and this may be associated with post-LASIK neurogenic inflammation,” explains Dr. Chao. In the absence of IVCM, the patient can be referred to an institute where IVCM can be conducted.
Takeaways
Remember that patients should always try to be treated for dry eye before any refractive surgery, regardless of what type will be used. Risk of developing post-op dry eye with neuropathic factors can be aided by IVCM. “While SMILE is an advanced refractive surgical technique, limited evidence indicates SMILE is superior to FS-LASIK in safety and performance. Therefore, patients should consult with their surgeon and optometrist about what the best option is,” Dr. Chao concludes.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
