 |
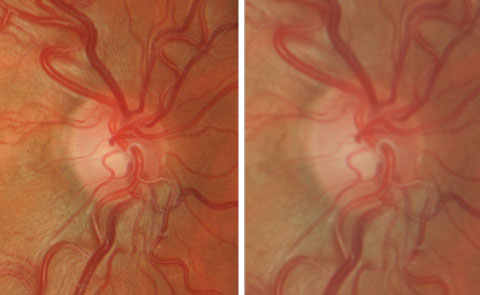
| Increased magnification (right) results in a “hazier” view. Click image to enlarge. |
The most commonly used lenses are indirect, also known as “aspheric” and “condensing” lenses, which are classically used at a slit lamp—for example, 78D or 90D lenses—or with a head mounted binocular indirect ophthalmoscope (e.g., 20D or 28D lenses). These are the traditional optics familiar to all eye care practitioners. They work very well and are available in a range of powers and designs.
Table 1. Indirect Lenses and Their Typical Use | ||
| Power | Purpose | Application |
| 90D | View the posterior pole using a slit lamp | Good general purpose lens. Alternative to 78D if the practitioner elects to use just one lens. |
| 78D | View the posterior pole using a slit lamp | Good all-around lens. Ideal option if thepractitioner uses a single lens. |
| 60D | View the posterior pole using a slit lamp | Ideal for optic nerve head examination as lens offers higher magnification near 1x. |
| 28D | View the retina including periphery using a head-mounted BIO | Lower magnification than 20D. Ideal for pediatric examination, when scleral indentation is required and for patients with nystagmus. Useful when slit lamp examination is not possible. |
| 20D | View the retina including periphery using a head-mounted BIO | Higher magnification than 28D. Ideal for pediatric examination, when scleral indentation is required and for patients with nystagmus. Useful when slit lamp examination is not possible. |
Slit lamp indirect ophthalmoscopy has become the standard diagnostic procedure for comprehensive eye examination. Volk Optical introduced the 60D lens in the early 1980s and, in subsequent years, extended the range of lenses for the slit lamp by adding additional powers. Over time, indirect ophthalmoscopy has come to replace the previously widespread use of direct ophthalmoscopy, and with good reason. Advantages include a larger field of view, a comfortable working distance between practitioner and patient, and most importantly a stereoscopic view, which enhances depth perception and helps provide a more comprehensive examination.
These lenses form a real, inverted image of the retina in between the lens and the practitioner. The technique is not always easy to master, but the benefits are notable once the user becomes proficient. Since the image is inverted and reversed, making a sketch of the retina on paper can be readily achieved by turning the page upside down and drawing what is seen, allowing for a simple conversion when the page is properly reoriented. Another tip for successful examination is to view the periphery sequentially and leave the macula until last, as taking patient comfort into account is likely to improve compliance.
Since the power of the optic dictates the magnification and field of view (see “Crunching the Numbers: Magnification and Field of View"), different lenses have distinct characteristics, which allow the doctor to select the best lens per their preference and the specific task to be addressed. Let’s consider their value for a variety of tasks.
Head-mounted BIO. When using the BIO, the type of condensing lens is as important as turning the light on. The advances in technology over the last few years have enabled a much more efficient and detailed examination of the retina, macula and optic nerve. Each has their advantages and disadvantages.
The main workhorse lens for use with the BIO is the 20D lens. This relatively low-powered lens (2.2D, 20D, Volk Optical; 20D Ocular Instruments; Diamond 20D Katena) is a compromise between magnification and field of view. Seeing subtle hemorrhages in the posterior pole with a red-free filter and analyzing peripheral retinal anomalies with scleral depression are its best qualities. It works best with a fully dilated pupil.
Advances in design have minimized reflections, allowing unobstructed views. Ocular Instruments has an attachment for its Maxfield 20D lens called the Saxena Retinal Grid 520, which fits onto the front side of the lens. It has a grid pattern of monofilament lines spaced at 5.20mm, which helps in estimating the size of retinal lesions, choroidal nevi and other anomalies in need of documentation by comparing the grid size with the optic nerve head. If a camera is not available, estimating the size with the grid provides a reliable measurement, which can be referenced at subsequent visits to rule out progression. Volk has developed a series of lenses with low dispersion glass and anti-reflective coating to further minimize reflections. The Digital ClearMag is designed to replace a 14/15D lens because of its increased magnification and the Digital ClearField is designed to replace a 20D/2.2 lens.
Crunching the Numbers: Magnification and Field of View | ||||||
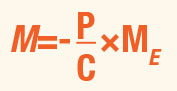
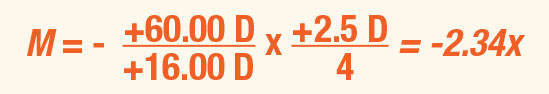
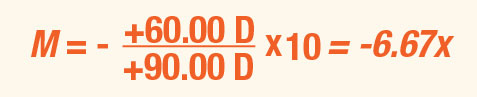
Indirect ophthalmoscopy is performed when the examiner views the image of a patient’s fundus through a condensing lens. Handheld lenses typically range in power from +14.00D to +40.00D, while condensing lenses included in a slit lamp may have a power as high as +120.00D. The resulting magnification is:
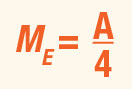
ME represents the amount of additional angular magnification needed for the examiner to clearly view the image produced by the condensing lens. ME is usually computed or quoted in reference to a standard viewing distance of 25cm (4D). The method of computing ME depends on how the examiner views the lens image. If the examiner performs handheld indirect ophthalmoscopy and has a sufficient amount of accommodation to view this image, then:
Consider a presbyopic examiner performing handheld BIO on an emmetropic patient. The examiner wears a +23.50D add. The refracting components of this patient’s eye (cornea and crystalline lens) may be modeled by a +60.00D thin lens. When the examiner holds a +16.00D condensing lens in front of the eye and views the image through the add, the magnification is:
If indirect ophthalmoscopy is performed with a slit lamp, then ME simply represents the amount of auxiliary magnification provided by the device. For example, consider the examiner viewing the emmetropic patient described above. She replaces the handheld condensing lens with a +90.00D lens in a slit lamp set at 10x magnification. The magnification in this scenario becomes:
Consider again the examiner performing handheld indirect ophthalmoscopy on an emmetropic patient with a +60.00D eye. The +16.00D condensing lens has a diameter of 50mm. The examiner holds this lens 7.26cm in front of the patient’s eye. The resulting field of view is:
|
The medium dioptric powered lenses (28D, 30D Volk Optical, 30D Ocular Instruments; Diamond 28D, Katena) are ideal for patients with small pupils or a constricted, opaque capsulorhexis opening of the anterior capsule following cataract surgery. They provide a larger field of view while sacrificing some magnification. You have to be even more discriminating when examining the fundus because of the lack of magnification. Ocular Instruments also has an attachment for its Maxfield 28D lens called the Saxena Retinal Grid 428, for help in estimating the size of lesion and nevi.
Very high-powered 40D lenses work well for retinal screenings, especially in patient populations where seeing into the eye is a challenge in itself. A large swath of retina can be seen at one time to rule out any obvious disease.
At the slit lamp. Typically, the 78D with 0.77x magnification is a versatile all-around lens; if practitioners are to own just one lens, this may well be the best choice. The 90D (0.64x) is an alternative option, as it too is an appropriate general-purpose lens. The 60D lens is especially suitable for disc imaging since it offers higher magnification of approximately 1x; the unit magnification also means that no conversion is required when measuring disc size. The 20D and 28D lenses are ideal when more magnification is required, or when a longer working distance is desired. These lenses are preferable when patients can’t work with the slit lamp, for children where a panoramic view is valuable and viewing time is limited, and for situations where imaging is challenging such as nystagmus or when scleral indentation is required (Table 1).
 |
| The medium dioptric powered lenses provide a larger field of view while sacrificing some degree of magnification. |
Selection factors. When choosing a lens, some of the key performance aspects to keep in mind include image quality, amount of light required, ease of imaging through the limiting pupil and the ergonomics of clinical use. Lens ergonomics specifically focus on the way it handles, the ease of control, the lens weight and general handling comfort. Much of this depends upon individual preference and previous experience. Traditionally indirect lenses have been made from glass and have a lens holder with knurling. This tried-and-true design is a favorite with many practitioners.
Some newer lenses have a different appearance, with a silicone grip (designed to improve lens control); these are more lightweight due to the materials used. The PMMA lens is lighter than a traditional glass lens and it is protected from scratches by a hard coating made of evaporated diamond.
Lenses for small pupils. New optical designs claim to improve imaging through small pupils, such as for patients whose pupils do not dilate well. Lenses from Katena use a steeper front surface to move the ray bundle forward into the pupil plane. This design is meant to be more efficient than designs that position the ray bundle further back in the eye, closer to the nodal point.
In practice, the efficiency in the illumination pathway means that lower light levels can be used during the examination. This may improve patient comfort and cooperation, particularly with children. Additionally, for those patients whose pupils do not dilate well—for example, individuals with diabetes or patients taking alpha-blockers such as tamsulosin—imaging the retina or at least the macula is usually still possible.
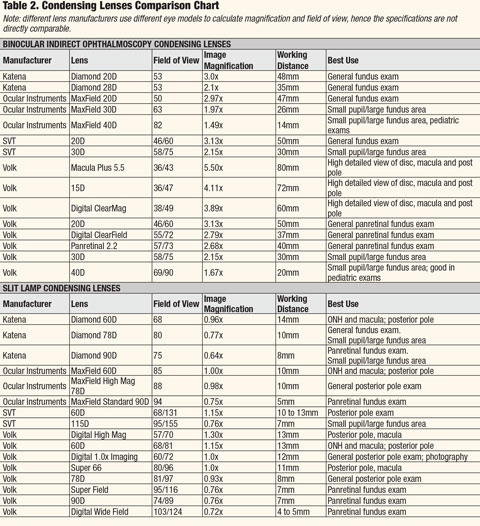 |
| Click table to enlarge. For PDF, click here. |
Fundus Biomicroscopy Lenses
These devices are essential in the evaluation of the optic nerve in glaucoma, maculopathy and peripheral retinal disease. After performing BIO and finding an anomaly, using condensing lenses designed for the slit-lamp allows for an “up-close” look at the condition.The optic nerve is best examined using a low-power biomicroscopy lens (e.g., 60D, Super 66 (66D), Volk Optical; 60D Ocular Instruments; Diamond 60D, Katena). Such a lens allows for greater magnification without having to use the high magnification of the biomicroscope, which results in a hazy view as the magnification of the slit lamp approaches the diffraction limits of light. Having a crisp image gives a detailed, clear view of the neuroretinal rim tissue that is vital in diagnosing and managing glaucoma.
 |
| The 20D lens is a good compromise between magnification and field of view. |
Peripheral fundus lesions are seen well with a high-powered biomicroscopy lens (e.g., 90D, SuperField, SuperVitreoFundus, Volk Optical; 90D, panfundus, Ocular Instruments; Diamond 90D, Katena). They allow the practitioner to see in great detail anomalies that may still be questionable after performing indirect ophthalmoscopy. The views possible from the BIO, scleral depression and the peripheral fundus lens gives the practitioner the information needed to make a specific diagnosis.
 |
| Use low dioptric power lenses for a clear, stereoscopic view of the macula, optic nerve and nerve fiber layer. |
Diagnostic Contact Lenses
While binocular indirect lenses offer significant benefits, another tremendously valuable way of imaging the retina is to use a contact diagnostic lens. Lenses such as Volk’s SuperQuad 160, Ocular Instruments Mainster PRP 165 or a Katena disposable Retina 180 provide access to even the most peripheral retina—a good view out to the ora serrata can be achieved. These lenses are surprisingly easy to use, assisted by the stability of the lens on the eye and more control over the eye and lids. While it is somewhat inconvenient to anesthetize the eye and use contact fluid, the imaging quality and access to ocular structures make the effort worthwhile.For the anterior segment, contact lenses are required to view the anterior chamber since the mirrors within the lens are required to overcome the cornea’s total internal reflection.
 |
| The Saxena Retinal Grid can help in estimating the size of lesions and nevi. |
An alternative to the customary 4-mirror lens is a 3-mirror lens. This one will access four different zones within the eye. Consequently, it is considered an “all-purpose lens,” as this device used on its own allows a comprehensive eye exam. It does take time to master the rotation of the mirrors along with movement of the slit lamp beam and the subsequent interpretation, but once achieved, this is an ideal lens for a thorough examination. This is evidenced by the 3-mirror lens remaining in routine eye care with minimal changes to the optics for the last 50 years.
Infection Control for Contact Lenses | |
| For lenses that touch the eye, there appears to be a trend towards disposable products. Both Volk and Katena offer single-use lenses in individual sterile pouches. They are popular in hospitals because of the time, cost and logistics of disinfecting traditional reusable lenses. The convenience of an immediately available sterile lens in a busy environment is very often welcome. With infection control always on the agenda in clinical environments, disposable medical devices have their place. Office-based practices may choose to use disposable lenses on “challenging” patients—for example, those with known hepatitis, HIV or a history of drug use. Practices may also benefit from the efficiencies in staff time and removal of disinfection chemicals. Single-use lenses are also a cost-effective way of trying a new type of lens without investing hundreds of dollars. |  Katena’s 4-mirror single-use gonio lens. Photo: Katena |
A broad selection of lenses is available to meet every clinical need and budget. These diagnostic and therapeutic lenses have stood the test of time, and the reusable style having been widely used over the last five decades. Lenses have recently undergone their own evolution due to modern manufacturing. This makes disposable lenses feasible and it is likely that they will become increasingly popular. Optometrists now have a wider range of lenses to choose from to address the various needs of their practices.
Dr. Pole is assistant professor at Michigan College of Optometry, where he teaches optics. He has no financial interests to disclose.
Dr. Walling is professor and director of continuing education at Michigan College of Optometry. He is has no financial disclosures relevant to this content.
Dr. Karpecki is the director of cornea and external disease at the Kentucky Eye Institute and Gaddie Eye Centers.
Dr. Karpecki is a consultant to Katena as well as manufacturers not relevant to this content.
Dr. Colatrella is the medical director and owner of PineCone Vision Center in St. Cloud, Minn. He has received honoraria from IOP Ophthalmics/Katena as well as manufacturers not relevant to this content.
Dr. Varanelli is an associate at the Simone Eye Center in Michigan, with a care emphasis on the medical and surgical comanagement of eye disease. He receives honoraria from Katena/IOP as well as manufacturers not relevant to this content.