42nd Annual Contact Lens ReportFollow the links below to read other articles from annual update on contact lenses: |
Despite today’s robust contact lens market, researchers continue to strive for the most comfortable and the healthiest lens possible, spending countless hours and resources improving oxygen content and lens tribology. “Tribology?” you may ask, unfamiliar with the term. The concept combines the more familiar notions of wettability, friction and lubricity when describing how two surfaces interact as they come into contact with each other. It is an apt way to think about the challenges inherent in contact lens wear. Lenses with a lower coefficient of friction may be associated with more end-of-the-day comfort, for example, and wetting agents are often incorporated into contact lens solutions to improve comfort.1
As the industry evolves and churns out newer lens options, clinicians sometimes struggle to understand which aspects of a lens will impact a patient’s success. To help, this article discusses oxygen permeability, water content, modulus and tribology, in regard to the lens lubricity and wetting angle, and how they are being implemented in the latest contact lenses.
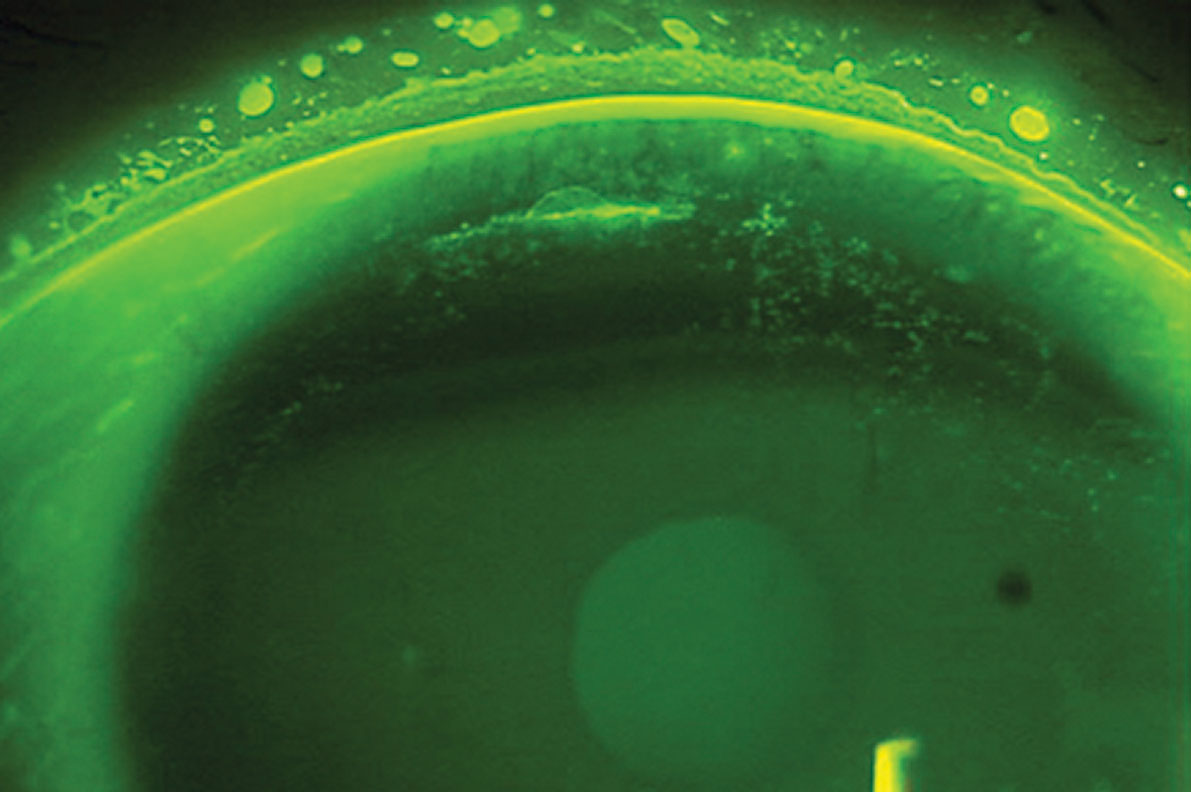 |
| Superior epithelial arcuate lesions, as seen here, can result from mechanical friction of a contact lens on the cornea and are mostly seen in those who wear high-modulus SiHy contact lenses. Click image to enlarge. Photo: Sruthi Srinivasan, PhD, BSOptom |
Oxygen Transmissibility
Dk/t, the unit of measurement for oxygen permeability through a contact lens, depends on the thickness of the lens. Re-evaluating the classic Holden-Mertz oxygen transmission values, researchers estimate that the average Dk/t required to preclude corneal hypoxic changes is 25 Fatt units to 30 Fatt units for daily wear lenses and 125 Fatt units for extended wear lenses.2
Unfortunately, clinicians rarely know the Dk/t values of the contact lenses they prescribe because labeling requirements do not mandate their inclusion. Contact lens manufacturers only provide the Dk/t of the center of a -3.00DS lens. This, however, is the thinnest portion of a minus lens, and the local Dk/t of the thickest portion of the lens should be evaluated instead, as this is the limiting factor for oxygen permeability.3,4
One study shows that limbal hyperemia is dependent on soft contact lens oxygen transmissibility in the lens periphery.5 Other researchers estimate that a peripheral Dk/t of 30 Fatt units or 40 Fatt units on a myopic contact lens should protect most corneas from developing neovascularization.6 As older HEMA contact lenses are replaced with silicone-hydrogel (SiHy) materials that have ever-expanding parameters and options, corneal hypoxia will hopefully become an issue of the past.
The latest SiHy contact lenses do not have as high of a Dk/t as the first generation SiHy lenses, but they have well-exceeded the minimum oxygen transmissibility values to prevent corneal hypoxia and more or less eliminated hypoxic stress.7 In addition, several studies document improved signs of hypoxia with decreased limbal hyperemia and end-of-the-day redness concurrent with rapid and sustained improvements in symptoms of comfort and dryness after patients were refit from HEMA to SiHy contact lenses.8-13
According to the Tear Film and Ocular Surface Society’s International Workshop on Contact Lens Discomfort, stricter experimental designs are needed to prove that oxygen permeability, not factors such as surface and bulk properties, increases contact lens comfort.1 Unfortunately, an experiment that controls for all lens factors may never be possible. Contact lens manufacturers, however, continue to diligently create new materials and designs to help improve lens comfort.
 |
| Controlling the Dk/t, wettability, friction and lubricity of a patient’s contact lens material can minimize lens issues, such as the contact lens-associated red eye pictured here. Photo: Ken Daniels, OD |
Water Content
The higher the water content in a contact lens, the more oxygen reaches the cornea during lens wear. HEMA lenses with lower water content have lower lens hydration and are more comfortable than their higher water content counterparts.14,15 This is because a HEMA contact lens with high water content loses moisture to the environment and absorbs water from the tears, potentially making the contact lens less comfortable.
For SiHy contact lenses, however, this association is not well-established; few studies correlate water content with lens comfort.1 We do know that the water content of SiHy lenses has increased from 24% to 74% over a 10-year period.16 This, combined with surface coatings, has led to a notable decrease in contact angle hysteresis, from greater than 40° in lotrafilcon A to less than 10° in delefilcon A.16 These advances have had a positive effect on our contact lens wearers; the less hysteresis, the more comfortable a lens is on the eye.
Measuring the Contact Angle HysteresisWhen using the Wilhelmy plate technique, a rectangular sample of contact lens material is immersed in and removed from a solution. The forces that the sample undergoes as it is lowered into and taken out of the liquid are recorded and used to calculate the contact angle. The advancing contact angle is measured as the sample is inserted in the solution, and the receding contact angle is found when the lens is removed from the liquid. The difference between the advancing and receding contact angles is known as the contact angle hysteresis.
|
Modulus
This refers to the flexibility of the contact lens, which can significantly impact a wearer’s success. The flexibility of the lens depends on the contact lens material, thickness and diameter.17 A softer material is generally considered more comfortable, and higher-modulus contact lenses are associated with poorer comfort, corneal staining, superior epithelial arcuate lesions, giant papillary conjunctivitis and mucin balls.18 However, lenses with a lower modulus can be difficult to handle, have limited eye movement and have altered optical performance from flexure.19
In HEMA lenses, the modulus directly correlates with the water content, which ranges from 30% to 80%.20
First-generation SiHy contact lenses originally had lower water content and higher modulus compared with HEMA lenses, making them stiffer. Second- and third-generation products decreased the amount of silicone and increased water content to improve lens comfort. Over a 10-year period, the silicone contact lens modulus decreased significantly, from 1.400MPa to 0.025MPa.16
The modulus of the latest generation of silicone contact lenses is now similar to the medium and high water content HEMA materials. Most of the studies that refit HEMA wearers into SiHy lenses report similar or higher levels of success, even when a lens with a high modulus was used.21
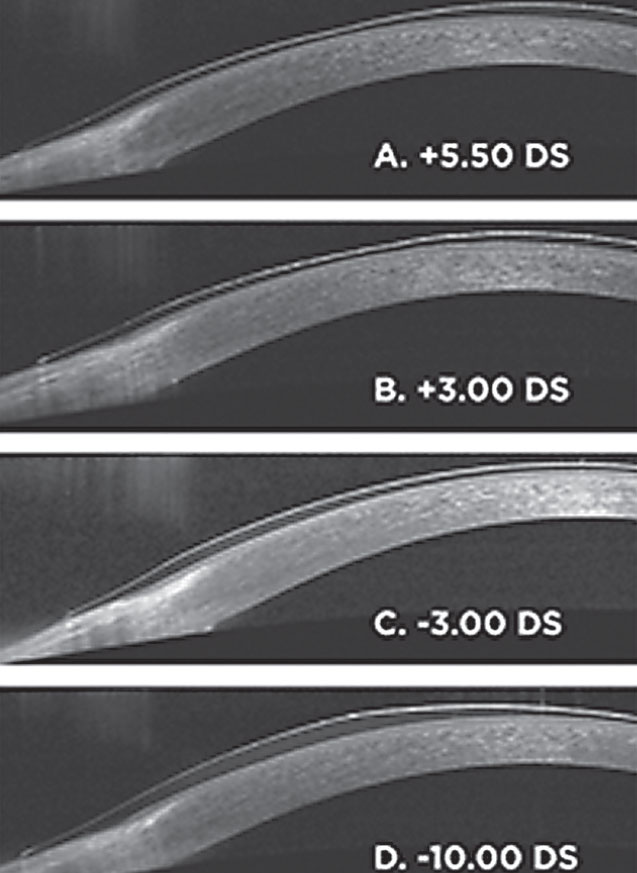 |
| Listed here are soft lens thickness profiles of various powers (A-D). Each image is half a spherical lens from the approximate optic center to the edge. The center thickness of the -3.00DS lens is 70µm. Photo: Aaron B. Zimmerman, OD, MS |
Friction and Lubricity
This is where the concept of tribology really comes to the forefront. Contact lenses that have little friction and a lower propensity for surface degradation have good lubricity.
The coefficient of friction is inversely correlated with contact lens comfort and can be lowered by adding surface coatings, plasma treatments or lubricants or by embedding bipolar surface-active agents—surfactants—into the lens material.1,22-24 One study found that an ultra-thin coating on a SiHy contact lens reduces surface friction and significantly improves comfort to levels achieved in patients not wearing contact lenses.23 A reduction of 0.025 in the friction coefficient—as measured by sliding a contact lens down an incline plane—is associated with a one-unit improvement on a comfort 10-point scale.22
The innate hydrophobic nature of silicone makes it necessary to add surfactants to lenses to increase their wettability and comfort.25 Surfactants, while initially introduced to aid in removing lipid deposits, also lower surface tension and increase wettability.26
Researchers are now developing compounds found naturally in the body, notably phosphorylcholine and albumin, to improve biocompatibility. These agents mimic membrane layers, minimize lipid deposition and reduce protein adsorption and inflammatory responses.27 Surfactants are also added to multipurpose contact lens solutions to maintain lubricity, control the signs and symptoms of dry eye and enhance the stability of the tear film.
Wettability
The degree to which the tear film can cover and maintain itself over a contact lens is important to successful lens wear but difficult to truly quantify.28 Ex vivo wettability is evaluated by finding the angle between the tear film and the contact lens; a wetter contact lens material has a smaller contact angle. Although many ways to measure contact angles exist, there is no standard technique. Thus, the measurements and units for a given material may vary between research groups.25
Overall, wetting angles alone are not sufficient to obtain a physically meaningful surface-wettability evaluation, and ex vivo results do not always correlate with in vivo comfort. Clinically, ex vivo wettability is often measured by the disruption of the tear film and the tear evaporation rate.29-31 While HEMA lens wettability is important in patients with dry eye, it is clinically indistinguishable in patients with a stable tear film.25
To improve the wettability of HEMA lenses, contact lens manufacturers may add wetting agents to blister packages and contact lens solutions. Common wetting agents include polyvinyl alcohol and hyaluronic acid, which are embedded in contact lenses and released from the lenses as they are worn throughout the day.
Because wetting agents embedded in HEMA lenses leach out over time, it is necessary to use a contact lens solution with wetting agents to uphold the lens wettability.32 Additionally, surfactants added to contact lens cleaning solutions increase the viscosity and lower the surface tension of the lens.26
Silicone-based contact lens wettability is dependent on the surface treatment of the lens in combination with wetting agents embedded in the lens matrix rather than wetting agents in the contact lens blister package. One study found that some SiHy contact lenses are actually more wettable than HEMA lenses, especially when soaked in a surfactant-free solution.32 Active surface agents in HEMA soft contact lenses leach out from the lens matrix and must be replenished by contact lens solutions with wetting agents.32
 |
| Click table to enlarge. |
Today’s Lens Options
The majority of recent-generation SiHy contact lenses contain modifications to improve comfort primarily by trying to boost wettability (Table 1). Here is a look at some of the latest lenses on the market that use extra wetting technology:
- Alcon’s Air Optix Aqua with Hydraglyde lens contains a plasma surface treatment and a surface wetting agent designed to create a hydrophilic surface that resists lens deposits, according to the company.33
- Alcon’s Dailies Total1 lens has a 33% water core wrapped in a gel-like outer layer that transitions to 80% at the surface and almost 100% water at the outermost surface of the lens.34
- Bausch + Lomb’s Ultra lenses contain a high concentration of wetting agent polyvinylpyrrolidone (PVP) on the lens surface.35 PVP is also distributed throughout the lens, allowing water to be stored within the matrix. This results in a relatively high water content of 46%.36
- Coopervision’s Biofinity lens combines two forms of silicone with hydrophilic monomers in a process that the company says makes additional wetting agents or surface treatments unnecessary.37
- Coopervision’s My Day lenses have the lowest amount of silicone (4.4%) compared with others in this class.38 According to the manufacturer, this allows for more space within the lens for hydrophilic materials, a 100Dk/t, a water content of 54% and a modulus of 0.40MPa.38
- Johnson & Johnson Vision’s Acuvue Oasys 1-Day lens distributes PVP evenly throughout the lens matrix in an attempt to replicate the properties of mucin as a means of improving the lens’ interaction with the tear film.26 The lens is also packaged in an electrolyte-balanced solution designed to mimic human tears.26
- Johnson & Johnson Vision’s Vita lenses use a combination of two modified silicones and, compared with Acuvue Oasys, 30% more PVP integrated throughout the lens matrix to improve hydration and comfort without needing surface treatments, according to the manufacturer.26
Comfort is Key
Contact lenses have many components that interact with one another in vivo on the eye, making what might feel like a simple process—fitting a contact lens—rather complicated. While extensive research into the various contact lens materials exists, more is needed to truly understand what makes the ideal contact lens. Fortunately, technology is moving in the right direction to allow for higher oxygen permeability, sustained lubricity and inherent wettability in lenses to maximize patient comfort and ocular health.
Dr. Yeung is a diplomate of the Cornea and Contact Lens section of the American Academy of Optometry and a senior optometrist at the University of California, Los Angeles (UCLA), Arthur Ashe Student Health and Wellness Center.
Ms. Dinh is an undergraduate in the biochemistry department at UCLA. She will graduate in June 2019.
1. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54:TFOS37-TFOS70. 2. Fonn D, Bruce A. A review of the Holden-Mertz criteria for critical oxygen transmission. Eye Cont Lens. 2005;31(6):247-51. 3. Bruce A. Local oxygen transmissibility of disposable contact lenses. CLAE. 2003;189-96. 4. Fatt I. New physiological paradigms to assess the effect of lens oxygen transmissibility on corneal health. CLAO. 1996;22(1):25-9. 5. Papas E. On the relationship between soft contact lens oxygen transmissibility and induced limbal hyperemia. Exp Eye Res. 1998;67:125-31. 6. Yeung KK, Yang HJ, Nguyen AL, et al. Critical contact lens oxygen transmissibility and tear lens oxygen tension to preclude corneal neovascularization. Eye Cont Lens. August 9, 2017. [EPub ahead of print]. 7. Wilcox MD. Microbial adhesion to silicone-hydrogel lenses: a review. Eye Cont Lens. 2013;39(1):61-6. 8. Dillehay SM. Does the level of available oxygen impact comfort in contact lens wear? A review of the literature. Eye Cont Lens. 2007;33(3):148-55. 9. Dumbleton K, Keir N, Moezzi A, et al. Redness, dryness and comfort following refitting long term low Dk hydrogel lens wearers with silicone-hydrogels. Optom Vis Sci. 2004;81(12S):31. 10. Chalmers R, Dillehay S, Long B, et al. Impact of previous extended and daily wear schedules on signs and symptoms with high Dk lotrafilcon A lenses. Optom Vis Sci. 2005;82:549-54. 11. Brennan N, Coles M, Comstock T, et al. A 1-year prospective clinical trial of balafilcon A (PureVision) silicone-hydrogel contact lenses used on a 30-day continuous wear schedule. Ophthalmology. 2002;109:1172-7. 12. Sickenberger W, Schmied I. Are new silicone-hydrogel contact lenses suitable for dry eye conditions in a daily wear mode? American Academy of Optometry International Program Book. Rockville, MD, American Academy of Optometry. 2002:161. 13. Long B, McNally J. The clinical performance of a silicone-hydrogel lens for daily wear in an Asian population. Eye Cont Lens. 2006;32:65-71. 14. Efron N, Brennan NA, Currie JA, et al. Determinants of the initial comfort of hydrogel contact lenses. Optom Vis Sci.1986;63:819-23. 15. Young G. Evaluation of soft contact lens fitting characteristics. Optom Vis Sci. 1996;73:247-54. 16. Tighe BJ. A decade of silicone-hydrogel development: surface properties, mechanical properties and ocular compatibility. Eye Cont Lens. 2013;39:4-12. 17. Brennan NA. New technology in contact lens materials. Trans Br Contact Lens Assoc Ann Clin Conf. 1988(11):23-8. 18. Alipour F, Khaheshi S, Soleimanzadeh M, et al. Contact lens-related complications: a review. J Ophthalmic Vis Res. 2017;12(2):193-204. 19. Tranoudis I, Efron N. Tensile properties of soft contact lens materials. CLAE. 2004;27(4):177-91. 20. Thompson TT. Tyler’s quarterly soft contact lens parameter guide. TQ. 2018;35(3):1-68. 21. Dumbleton K, Keir N, Moezzi A, et al. Objective and subjective responses in patients refitted to daily-wear silicone-hydrogel contact lenses. Optom Vis Sci. 2006;83:758-68. 22. Kern J, Rappon J, Bauman E, et al. Assessment of the relationship between contact lens coefficient of friction and subject lens comfort. IOVS. 2013;54: E-Abstract 494. 23. Vidal-Rohr M, Wolffson J, Davies L, et al. Effect of contact lens surface properties on comfort, tear stability and ocular physiology. CLAE. 2018;41(1):117-21. 24. Schmidt T, Sullivan D, Knop E, et al. Transcription, translation, and function of Lubricin, a boundary lubricant, at the ocular surface. JAMA Opthalmol. 2013;131(6):766-76. 25. Svitova T, Lin M. Wettability conundrum: discrepancies of soft contact lens performance in vitro and in vivo. Eur Phys J Spec Top. 2011;197:295-303. 26. Keir N, Jones L. Wettability and silicone-hydrogel lenses: a review. Eye Cont Lens. 2013;39(1):100-8. 27. Kemsley J. From pexiglas to silicone-hydrogels-the materials that let you see through the other side. Chem Engin News. 2008;86(11):47. 28. Maldonado-Codina C, Morgan PB. In vitro water wettability of silicone-hydrogel contact lenses determined using sessile drop and captive bubble techniques. J Biomed Mater Res A. 2007;83:496-502. 29. Thai LC, Tomlinson A, Doane MG. Effect of contact lens materials on tear physiology. Optom Vis Sci. 2004;81:194-204. 30. Nichols JJ, Mitchell GL, King-Smith PE. Thinning rate of the precorneal and prelens tear films. Invest Ophthalmol Vis Sci. 2005;46:2353-61. 31. Craig JP, Tomlinson A. Importance of the lipid layer in human tear film stability and evaporation. Optom Vis Sci.1997;74:8-13. 32. Lin MC, Svitova TF. Contact lens wettability in vitro: effect of surface-active ingredients. Optom Vis Sci. 2010;82:440-7. 33. Air Optix. Air Optix SmartShield technology. www.airoptix.com/contact-technology.shtml#ultra-smooth. Accessed July 17, 2018. 34. Alcon. Dailies Total 1 water gradient contact lenses. www.myalcon.com/products/contact-lenses/dailies/dt1-technology.shtml. Accessed July 17, 2018. 35. Bausch + Lomb. Bausch + Lomb Ultra contact lenses. www.bausch.com/ecp/our-products/contact-lenses/myopia-hyperopia/bausch-lomb-ultra-contact-lenses. Accessed July 17, 2018. 36. Steffen R, Hook D, Schafer J, et al. New technology yieldsdehydration resistance. Paper presented at the American Academy of Optometry, November 14, 2014; Denver, CO. 37. Coopervision. Smart Silicone chemistry. coopervision.com/practitioner/our-products/contact-lens-technology/smart-silicone-chemistry. Accessed July 17, 2018. 38. Coopervision. My Day. coopervision.com/practitioner/our-products/myday/myday. Accessed July 17, 2018. |

