 |
Whenever encountering glaucoma in practice, we immediately strive to employ an effective treatment regimen to preserve visual function. This is a critical and necessary goal, but, as primary care practitioners, there is often more to the story. Determining the cause of glaucoma, for example, may alter your overall management approach. Specifically, secondary glaucomas such as pseudoexfoliative are important to distinguish from other forms because it further requires systemic evaluation. To understand why, we must visit the pathogenesis of this systemic syndrome.
Genetic Considerations
Pseudoexfoliative syndrome (PEX) is a systemic disorder that manifests primarily in the eye, particularly in structures of the anterior segment. It is distinct from true exfoliation, which is a result of infrared damage affecting the anterior lens capsule. One well-established link for the development of PEX is the LOXL-1 gene at locus 15q22. This gene codes specifically for elastic fiber constituents of the extracellular matrix.1
To understand the impact of this alteration, we have to revisit the function of elastic fibers. Elastin is an extracellular matrix connective tissue protein responsible for the elasticity and recoil of various structures and organs throughout the body. Included in its effects are large arteries, the heart, pulmonary structures, skin and eyes. Under normal and healthy conditions, this complex structure slowly degrades over time, with a half-life of 70 years due to its intricate network of crosslinked components. Tropoelastin is a soluble precursor for elastic fibers, responsible for promoting the attachment and migration of various molecules such as fibroblasts, endothelial cells and others. It is the most elastic protein molecule, with the ability to stretch eight times its original length, and is bridged and crosslinked by the enzyme lysyl oxidase (LOX) to form a mature fiber. This explains the relationship between extracellular matrix elastin and tropoelastin as well as the role of LOX—all of which are mechanisms implicated in the pathophysiology of PEX.2
 |
|
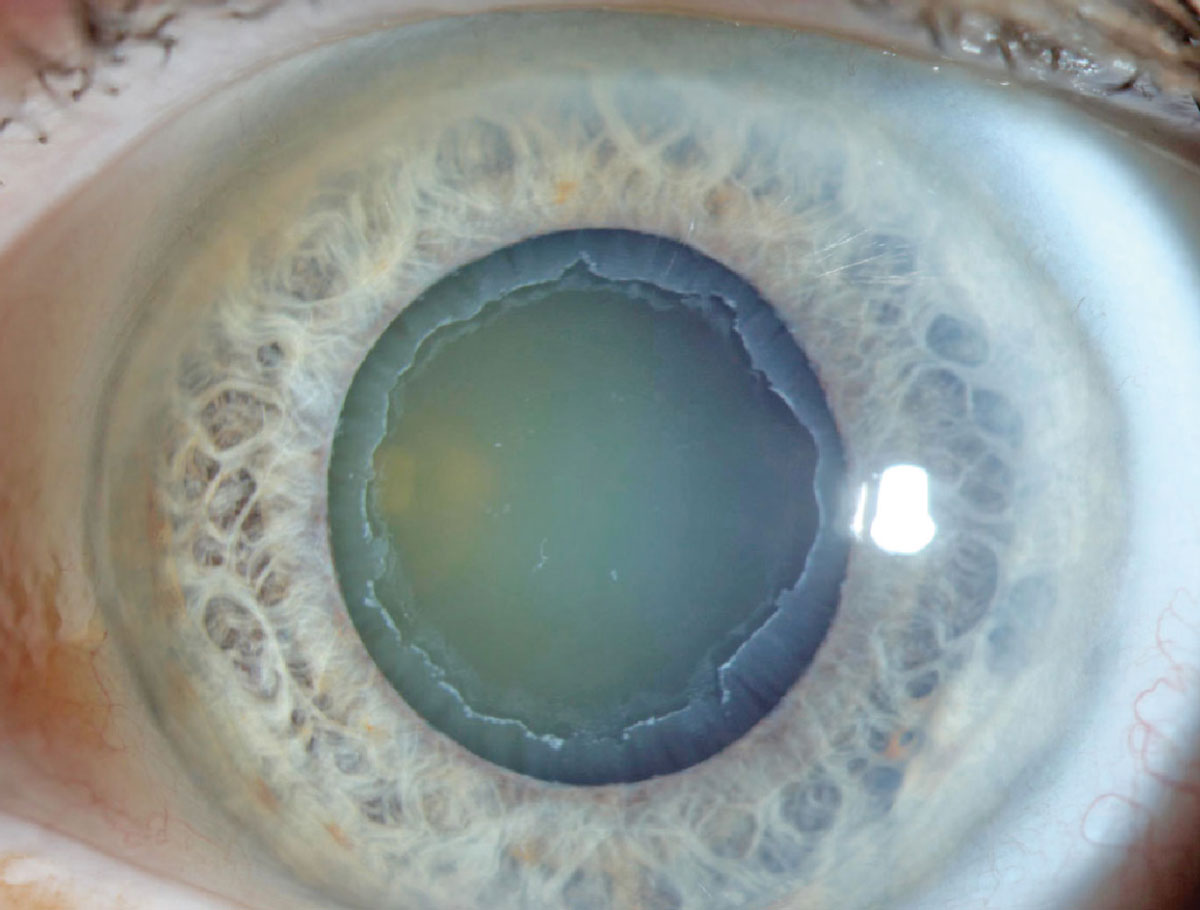
PEX can cause notable effects to the cornea and iris. Photo: Aaron Bronner, OD. Click image to enlarge. |
Elastin is abundant throughout the body in elastic structures. This includes, but is not limited to, the aorta and major blood vessels such as large arteries, the lungs, elastic ligaments, tendons, the skin, liver and eyes.2 As such, PEX is not an ocular condition but a systemic one. However, it does predominantly affect the structures of the eye and can be diagnosed through an ocular examination. As mentioned, this is likely due to elastic fibers being integral in maintenance of ocular structures. In fact, elastin is present throughout many ocular structures, such as the conjunctiva, muscle tendons, sclera, choroid and meninges. Most importantly, it is densest in the sclera surrounding the peripapillary optic nerve head. One can surmise the relationship between PEX and glaucoma from this anatomic information alone.3
Clinical Ramifications
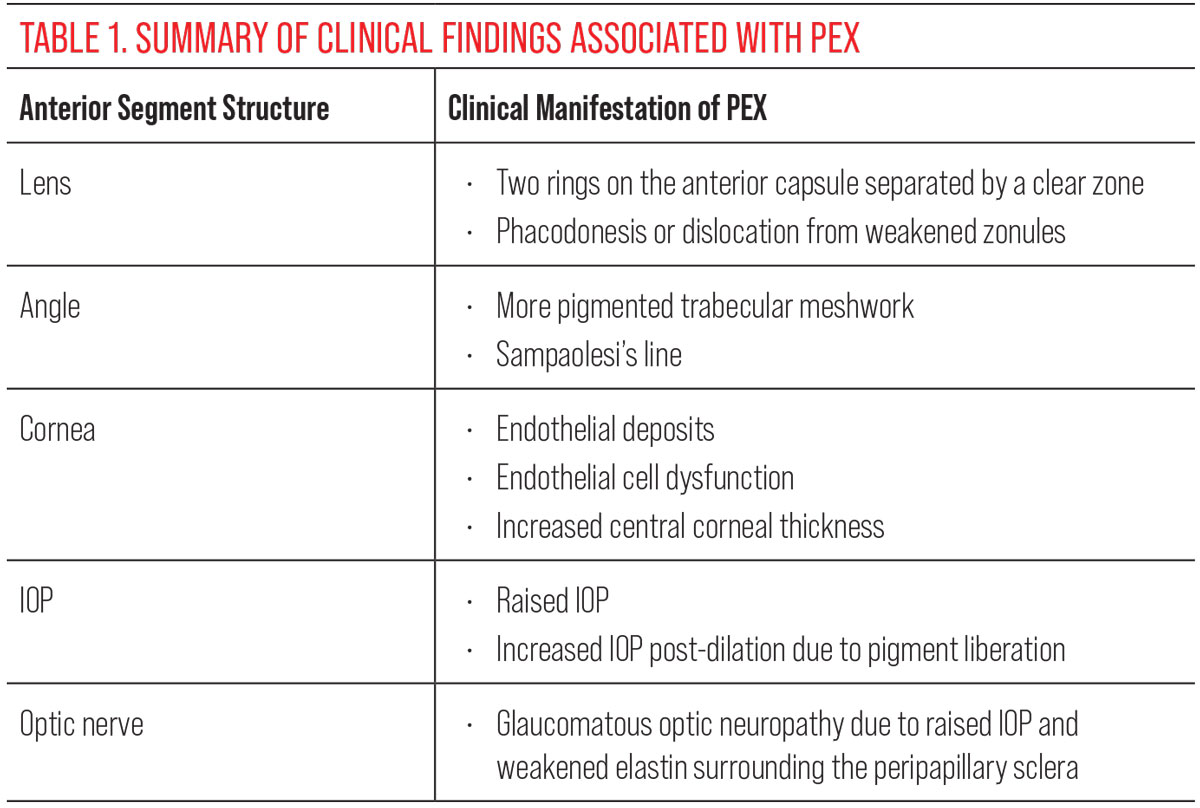
A defect in the elastin and lysyl oxidase relationship yields the production of aggregated protein deposits, or exfoliative material, in tissues that synthesize elastin fibers. As this relates to the eye, these depositions accumulate in the ciliary body, anterior lens capsule, iris and trabecular meshwork. All these areas are necessary for aqueous production, circulation and drainage to prevent an increase in intraocular pressure (IOP) and subsequent development of glaucoma. Clinical findings on ocular examination may include the following structures:
- Lens. Easily the most common diagnostic feature is the deposition of material on the anterior surface of the lens, comprising three zones. The first is a central ring corresponding to the diameter of the patient’s normal pupil size. The outermost ring is a granular, layered peripheral margin. Separating these two areas is a third clear zone. The lens can also become weakened over time from damage to the zonules, called phacodonesis. This not only can cause lens dislocation but also can complicate cataract surgery techniques.
- Iris. Findings of this structure can overlap with a different type of secondary glaucoma—pigmentary dispersion glaucoma (PDS). In PEX, exfoliative material can accumulate around the pupillary border. There is also loss of pigment around the sphincter, leading to iris transillumination defects. Iris blood vessels are also narrowed to a greater degree or destroyed.
- Trabecular meshwork. Also overlapping with PDS, there is often increased pigmentation of the trabecular meshwork with PEX, as well as pigmented Schwalbe or Sampaolesi line.
- Cornea. Evidence of PEX can also be found on the cornea in the form of exfoliative buildup on the central corneal endothelium. The endothelium also often exhibits cellular dysfunction because of cellular loss, leading to an increase in corneal thickness.
- IOP. The marked increase in IOP is what makes PEX patients significantly more susceptible to developing glaucoma. The material deposited into the trabecular meshwork prohibits the free flow of aqueous. Oftentimes, there will be an increase in post-dilation IOP due to additional pigment liberation from dilation.1,3,4
 |
| Click image to enlarge. |
Holistic Care
The astute clinician can readily recognize PEX and knows to look for evidence of it, either treating the patient for glaucoma or to monitor them for their increased susceptibility in its development upon PEX manifestation. Keep in mind, though, that the eye is not the only site of pathology, as elastic fibers are present at various sites throughout the body. Several well-known studies have identified a correlation between patients who have ocular manifestations of PEX, including glaucoma, and a positive association with hypertension, myocardial infarction, stroke, angina and aortic aneurysms. Elevated homocysteine levels, which are implicated in cardiovascular diseases, is another potential correlation. The vast number of elastic fibers in the structures of the heart is key in substantiating these claims.4
Though the mechanism of PEX is extremely complex and multifaceted, this oversimplification of its pathophysiology is helpful in being able to appropriately manage your patient. Because of PEX’s primarily ocular manifestations, the eyecare provider is key in diagnosing the syndrome, monitoring and treating the ocular sequelae and in corresponding with the patient’s primary care and other providers to manage systemic risks.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Ariga M, Nivean M, Utkarsha P. Pseudoexfoliation syndrome. J Curr Glaucoma Pract. 2013;7(3):118-20. 2. Wang K, Meng X, Guo Z. Elastin structure, synthesis, regulatory mechanism and relationship with cardiovascular diseases. Front Cell Dev Biol. 2021;9:596702. 3. Gelman S, Cone FE, Pease ME, et al. The presence and distribution of elastin in the posterior and retrobulbar regions of the mouse eye. Exp Eye Res. 2010;90(2):210-5. 4. Vardhan AS, Haripriya A, Ratukondla B, et al. Association of pseudoexfoliation with systemic vascular diseases in a South Indian population. JAMA Ophthalmol. 2017;135(4):348-54. |

