 |  |
Angioid streaks—defects in Bruch’s membrane—can cause visual disturbances in multiple ways.1 The streaks may traverse the fovea, leading to retinal pigment epithelium (RPE) disruption. In addition, mild trauma to the eye may cause the choroid to rupture at these areas, leading to submacular hemorrhage. Secondary choroidal neovascularization is also possible.
Angioid streaks have many systemic associations, as summarized by the ‘PEPSI’ mnemonic: Pseudoxonthoma Elasticum, Paget’s disease, Sickle-cell/thalassemia/spherocytosis, Idiopathic. Of note, Ehlers-Danlos syndrome, once part of the mnemonic, is no longer commonly believed to be associated with angioid streaks.2
Pseudoxanthoma elasticum is an inherited multi-system disorder characterized by ectopic mineralization and fragmentation of elastic fibers in the skin, the elastic laminae of blood vessels and Bruch’s membrane in the eye.3 Defects in an ATP-binding cassette (ABC) transporter gene in ABCC6 on chromosome 16 are responsible for the disease.4
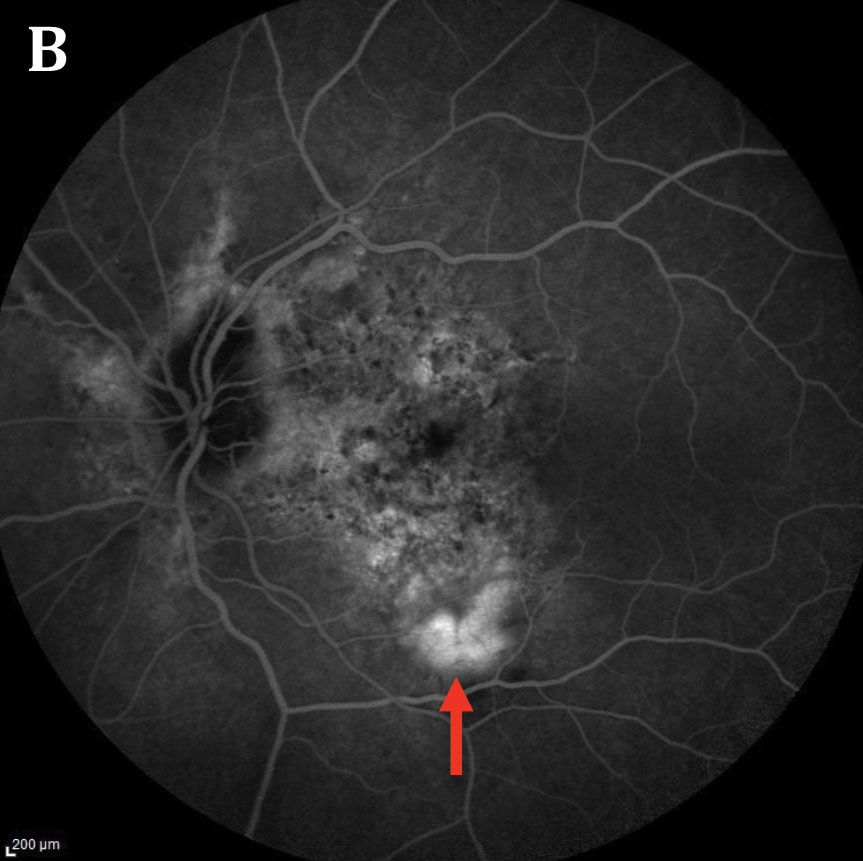
In addition to angioid streaks, other ophthalmic manifestations of this disease include a ‘peau d’orange’ fundus appearance, which may appear as mottled dark spots on a lighter background.
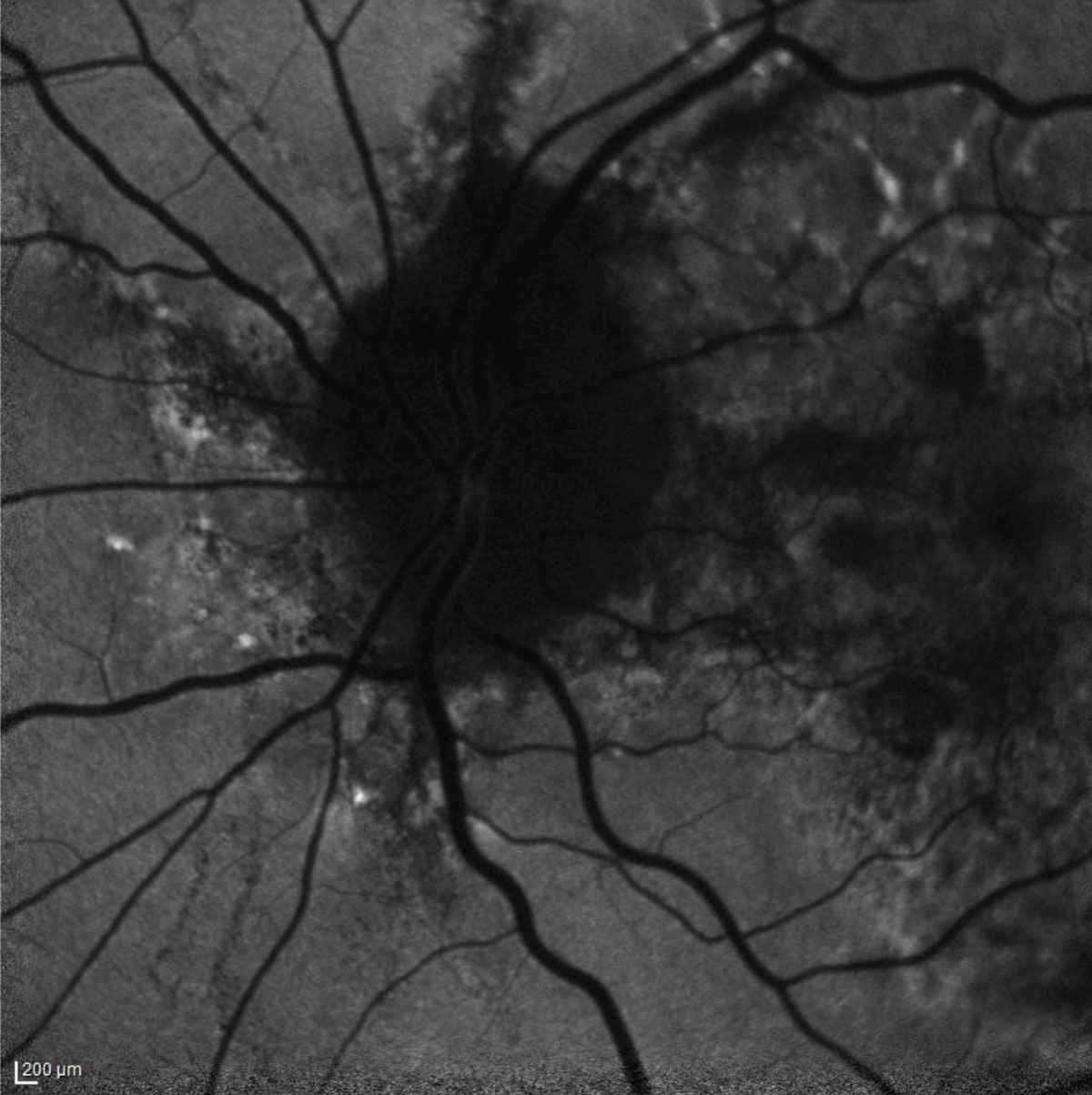 |
| Fig. 1. The patient’s fundus autofluorescence demonstrates hyperfluorescent streaks radiating from the optic nerve that correspond clinically with angioid streaks. Click image to enlarge. |
On a Losing Streak
Case by Drs. Haynie and Banda
A 57-year-old female presented with a one-week history of a painless distortion in the left eye. She describes seeing a ‘wave’ near the center of her vision. She stated that she had similar symptoms in her right eye several years ago and was treated for wet age-related macular degeneration. She denies any major medical problems. Her 12-point review of systems was otherwise negative, other than skin changes for most of her adult life.
Her best-corrected visual acuity was 20/40 in right eye and 20/50 in the left eye. No relative afferent pupillary defect was noted. Confrontation visual fields and extraocular motility were intact. Her anterior segment examination was otherwise unremarkable.
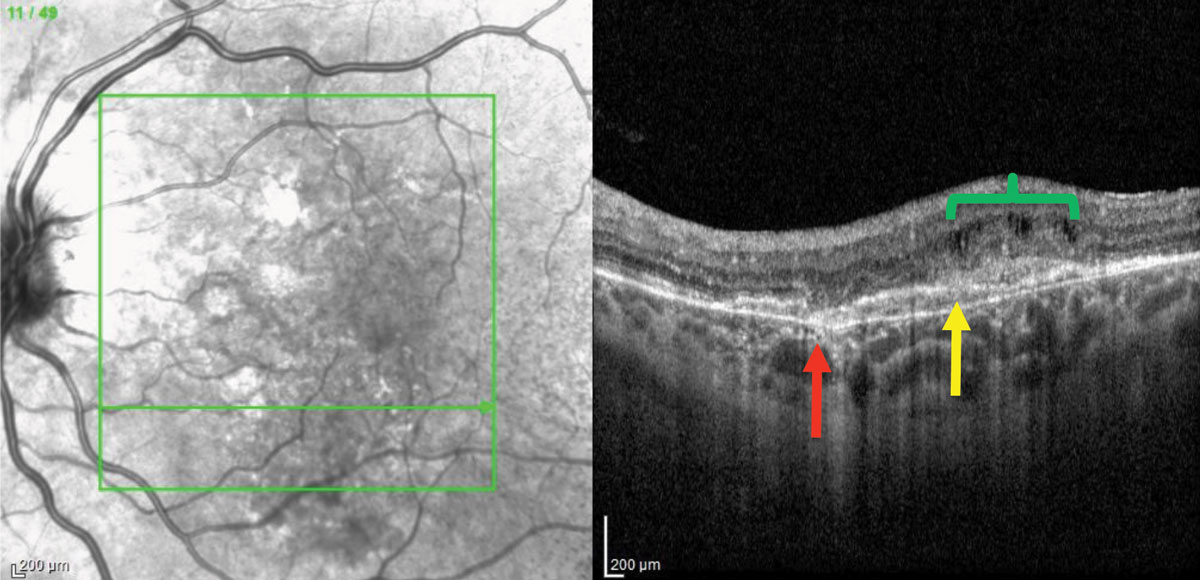 |
| Fig. 2. OCT of the left eye demonstrates a break in Bruch’s membrane (red arrow), a shallow pigment epithelial detachment with overlying subretinal hyper-reflective material (yellow arrow) and cystoid macular edema (green bracket). Click image to enlarge. |
The dilated fundus examination revealed orange-red linear irregularities extending radially from the optic nerve into the peripheral fundus in both eyes. These linear changes were better visualized on fundus autofluorescence (FAF), more obviously demarcated in the left eye (Figure 1). Spectral-domain optical coherence tomography (SD-OCT) of the right macula revealed changes such as RPE irregularities; however, no intraretinal or subretinal fluid was noted. In the left eye, SD-OCT showed a break in Bruch’s membrane, sub-retinal hyper-reflective material and associated intraretinal fluid (Figure 2). Fluorescein angiography (FA) of the right eye showed a perifoveal lesion with early hyperfluorescence and late leakage, consistent with a choroidal neovascular membrane (CNVM) (Figure 3).
The patient was diagnosed with angioid streaks and a new choroidal neovascular membrane in the left eye. She had characteristic skin findings on her neck consistent with the diagnosis of pseudoxonthoma elasticum (Figure 4). The patient elected for treatment with anti-VEGF agents in the left eye.
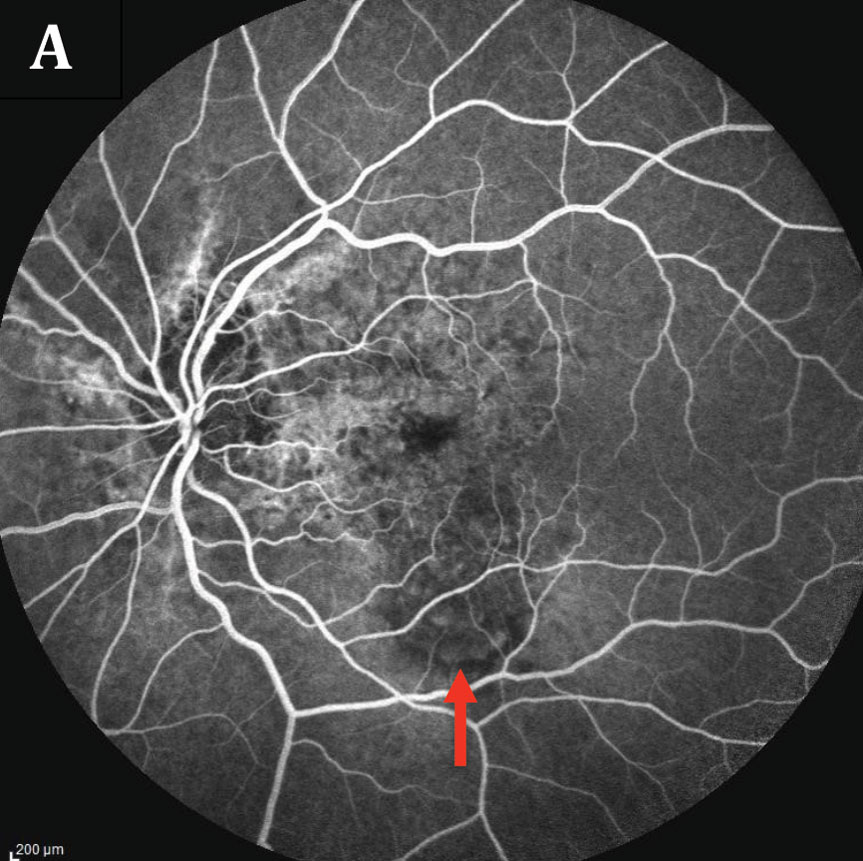 |  |
| Fig. 3. The patient’s fluorescein angiography of the left eye (A) shows early hyperfluorescence noted inferior to fovea with late leakage (B). Angioid streaks surrounding the nerve can also be seen as staining. Click images to enlarge. | |
Shifting Focus
Commentary by Dr. Shechtman
Angioid streaks are bilateral blood vessel-like cracks emanating from the optic nerve. Although angioid streaks can be idiopathic, there is often an underlying cause, which the driving force when managing these patients.
Clinicians must determine the presence of such etiologies, as well as address the ocular complications. System workup may be specific based on the clinical presentation, such as the case provided. The three most frequently encountered systemic associations are pseudoxonthoma elasticum, Paget’s disease of bone and sickle cell hemoglobinopathies; thus, workup should focus first on these conditions.
Optometrists should communicate with the patient’s primary care provider to ensure the patient receives the proper testing. Along with a complete comprehensive medical exam, the primary care provider should consider a skin biopsy, serum alkaline phosphatase/calcium/phosphate and hemoglobin electrophoresis, among other testing when necessary.
 |
| Fig. 4. A color photo of the patient’s skin findings associated with pseudoxanthoma elasticum depicts the ‘peau d’orange’ appearance. Click image to enlarge. |
As for treatment, angioid steaks are merely observed for secondary complications such as CNVM. Both FA and SD-OCT are helpful tools used to assess these complications. Clinicians should ask patients to follow a home Amsler grid and return to the clinic if they experience any new visual symptoms. CNVM is typically treated with standard anti-VEGF therapy.
Of note, common differentials include lacquer cracks, choroidal rupture and streaks seen in patients with histoplasmosis. Careful evaluation using FA, FAF or red-free photography, in addition to correlating history (i.e., history of trauma) and location (presence of white streaks near the macula in a high myope), helps to reveal the proper diagnosis.
1. Georgalas I, Papaconstantinou D, Koutsandrea C, et al. Angioid streaks, clinical course, complications, and current therapeutic management. Ther Clin Risk Manag. 2009;5(1):81-9. 2. Singman EL, Doyle JJ. Angioid streaks are not a common feature of Ehlers-Danlos syndrome. JAMA Ophthalmol. 2019;137(3):239. 3. Gliem M, Zaeytijd JD, Finger RP, et al. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front Genet. 2013;4:14. 4. Chassaing N, Martin L, Calvas P, et al. Pseudoxanthoma elasticum: a clinical, pathophysiological and genetic update including 11 novel ABCC6 mutations. J Med Genet. 2005;42:881-92. |

