From comparisons of the latest high-tech equipment to research on medications, this years Association for Research in Vision and Ophthalmology (ARVO) meeting had something of interest to anyone with an interest in glaucoma. The past 10 years have witnessed major clinical advances in the study of this mysterious yet very treatable disease, and that trend appears to be ongoing.
With data from the Ocular Hypertension Treatment Study (OHTS) released two years ago, central corneal thickness remains a popular research topic. Investigations also looked at other methods to better understand glaucoma risk factors, as well as comparisons of new technology and insights into diagnosis and treatment of the disease.
Central Corneal Thickness
Central corneal thickness was weakly related to progression of visual field loss but not to optic-disc changes, according to a study out of Dalhousie University in Canada.958 The study consisted of 82 eyes of 43 patients (mean age of 55.9 years and mean follow-up of 9.8 years). Researchers examined visual fields with a Humphrey 30-2 program and optic discs with a Heidelberg Retinal Tomography every six months, and measured corneal thickness using ultrasound pachymetry. Progression was determined using a trend analysis that yielded values between 0 (no evidence of progression) to 16 (very high evidence). The trends were weak but consistent, and appeared to be independent of intraocular pressure.
Are eyes with thinner corneas more susceptible to glaucomatous damage? A multi-center U.S. study looked at 41 subjects with asymmetric glaucoma, which researchers defined as cup-to-disc ratio asymmetry greater than 0.2.936 The eye with the larger cup-to-disc ratio also had the thinner cornea in 34 out of the 41 pairs of eyes, a statistically significant link. This raises the question: Is the cornea a biological indicator of glaucoma in some susceptible eyes?

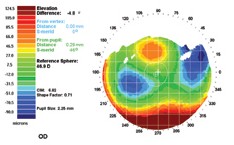
Patients with open angle glaucoma, as in this eye, were tested with a combination of travoprost and timolol. The combination lowered IOP more than either agent alone.
More evidence that African decent is a risk factor for thin corneas was produced by a SUNY Downstate paper.4493 Researchers divided 145 patients into three groups: blacks, Caribbean Islanders and whites. Ethnicity proved a significant factor in predicting corneal thickness. Mean corneal thickness was 586m for whites, 525m for blacks, and 507m for Caribbean Islanders. The difference between the latter two groups was not statistically significant, but when both were compared with whites the difference was significant. Researchers speculated that structural characteristics associated with a thin central cornea may predispose patients to primary open angle glaucoma.
Medications
A new drug combination of travoprost and timolol appears to be well tolerated and reduces IOP more effectively than either agent alone, according to a paper from the University of Washington and Alcon Research, Fort Worth, Texas.2113
Patients with open angle glaucoma or ocular hypertension randomly received either combination travoprost 0.004%/timolol 0.5%, travoprost 0.004% alone, or timolol 0.5% alone, and were followed for three months. In the 258 patients enrolled, the combination solution produced significantly lower IOPs than timolol, with a mean IOP difference in favor of the combination solution ranging from 1.9-3.3mm Hg. The mean difference in favor of the combination solution over travoprost was 2.0-2.4mm Hg at the crucial 8 a.m. time point. No safety concerns were noted.
Discontinuing nasal steroids in patients with glaucoma or ocular hypertension leads to a clinically significant drop in IOP, according to a Vanderbilt University study.945 Researchers reviewed the charts of 13 glaucoma and ocular hypertension patients with elevated or suboptimal IOPs who were taking nasal steroids. Mean IOPs were 14.5mm Hg before steroid usage, 17.5mm Hg during usage, and 13.8mm Hg post-usage. None of the patients were aware that the nasal sprays were steroids. Also, two of the subjects were known steroid responders. Of the 26 eyes, 21 had a mean 19% IOP decrease once steroids were discontinued for a mean 42 days. Given the impact of steroids and the low level of awareness among patients, the researchers suggested inquiring about use of nasal sprays during patient history.
Contrary to popular assumption, patients on once-a-day medications do not appear to be any more compliant than those on twice-a-day drugs, according to an Indiana University study.4510 Eighty patients were divided into those on once-a-day glaucoma medications and those on twice-a-day medications, and researchers monitored refill data at the subjects pharmacies. If patients refilled their prescriptions as directed, their compliance was rated 100%. If they refilled their medications less or more frequently than their dosage required, their compliance was rated below or above 100% accordingly. Allowing some dosing variations, researchers deemed a score of 85%-115% to be compliant. Once-a-day patients exhibited a 25% over-utilization rate and a 37.5% under-utilization rate. Twice-a-day patients exhibited a 30% over-utilization rate and a 27.5% under-utilization rate. None of these compliance rates were significantly different.
A thin cornea, such as this, may be more susceptible to glaucomatous damage.
Changes in systemic blood pressure appear to be associated with changes in IOP and vice versa, a University of Wisconsin study concludes.3413 Investigators looked at 4,926 people between the ages of 43 and 86 between 1988 and 1990. Researchers measured blood pressure and IOP, and repeated the process five years later. Thirty-four percent of the subjects were on anti-hypertensive medication at baseline, and most of those patients were on the same medications at the second exam; 12% took such medications only at the second exam. These medications were associated with variations in blood pressure and IOP, with a decrease of about 0.20mm Hg in IOP for a decrease of 10mm Hg systolic blood pressure and a decrease of about 0.50mm Hg in IOP for a decrease of 10mm Hg diastolic blood pressure.
Diagnostic Instruments
Three studies compared various methods of viewing the optic nerve. A German team compared the Stratus optical coherence tomography (OCT) and the Heidelberg Retina Tomograph (HRT).3333 The study looked at 86 eyes: 31 healthy, 36 with moderate and 18 with primary open angle glaucoma. Rim volume (RV), disc area (DA), cup area (CA), rim area (RA), and cup-to-disc area ratio (CD) were calculated using both devices. OCT measurements were taken using two cup offsets: 0 and 150m. In most measurements, OCT and HRT correlated in both normal and glaucoma patients. However, in normal patients, RA and RV did not correlate. Researchers suspected that a cup offset somewhere between 0 and 150m might provide a better concordance between the two device measurements.
A study out of Korea evaluated the relationship between the optic disc measurements generated by confocal scanning laser ophthalmoscopy (CSLO) and OCT.3315 Researchers scanned 52 eyes in 27 non-glaucomatous patients with CSLO-TopSS and OCT-OCT 3000. The measurements from both devices were highly correlated, except in eyes with tilted discs. In eyes with a disc tilt of more than 4 degrees, the disc area and neuroretinal rim area were larger and the cup-to-disc ratio was smaller when measured by the OCT. But regardless of tilt, the cup area showed no difference between the two devices.
A new fundus camera technique was compared to HRT measurements in a Canadian study.3344 Disc areas from fundus photographs taken with a Nidek non-mydriatic camera were measured in pixels using Adobe Photoshop 7.0 and a magnification factor determined employing a technique in which the position of the focusing knob on the camera accounts for the refractive error. This simple method was described in a 2003 issue of the Archives of Ophthalmology (2003;121:707-709). Regression analysis correlated strongly the technique with the HRT measurements, which prompted researchers to advocate its use in population-based, mass glaucoma screenings.
A German study found that OCT corneal pachymetry was more accurate than ultrasound pachymetry.4494 Researchers compared the Pachette 500 ultrasound pachymeter to the OCT device made by 4optics, a German company. The ultrasound device produced higher values of central corneal thickness. The OCT standard deviation was smaller by 6m in the right eyes and 4m in the left eyes, researchers found.
Early Detection
Studies at this years ARVO meeting looked at the ability of diagnostic devices to detect glaucoma damage. A research team at Jules Stein Eye Institute found that OCT could effectively discriminate between glaucoma suspects and patients with disc damage.948 The study consisted of 36 patients who were diagnosed as glaucoma suspects or as having early glaucoma. The researchers found that average nerve fiber layer thickness was 98.7m in glaucoma suspects, and 85.5 microns in patients with disc damagea significant difference.
A University of California study found that HRT Moorfields classification may be predictive of field loss on short-wavelength automated perimetry (SWAP).3305 Researchers followed 173 glaucoma suspects with normal SWAP and standard visual fields and found that the strongest univariate predictor of repeatable SWAP damage was HRT Moorfields Regression analysis (MRA) classification in the temporal superior region. Larger studies are needed to confirm these findings, researchers stated.

OCT can discriminate between glaucoma suspects and patients with disc damage.
Meanwhile, an Israeli study found the GDx Nerve Fiber Analyzer with variable corneal compensator (VCC) had a high sensitivity and moderate high specificity for diagnosing glaucoma damage.3325
Frequency doubling technology (FDT) appears to detect visual field progression earlier than standard automated perimetry (SAP), a Canadian study finds.3472 One eye in each of 71 patients with open-angle glaucoma was tested every six months with both FDT and SAP for a median duration of four years. In those patients classified as progressing by both FDA and SAP, FDT detected the progression earlier.
Patients with abnormal FDT results exhibited a high risk of developing scotomas three years later, according to a multi-center Japanese and British study.2129 Eighty eyes of 42 patients with glaucoma or suspected glaucoma were followed for up to three years. The central 58 test points in HFA were assigned to one of the 17 clusters corresponding to FDT test points. Even in cases in which the baseline score was normal, an abnormal result in baseline FDT showed a high risk of future scotoma as measured by HFA three years later.
Glaucoma suspects with asymmetric disc sizes may be less likely to have glaucoma than subjects with symmetrically sized discs, concludes a Canadian study.5543 Disc asymmetry can occur in subjects whose optic canal in one eye is significantly larger than the fellow eye, but in whom the neuroretinal rim area is equal. Such eyes may be misdiagnosed as glaucoma cases. Investigators took digital images of the optic nerve heads of 116 subjects. In subjects whose disc size difference was greater than 10%, the mean visual field defect was -2.28dB. In subjects whose disc size difference was less than 10%, the mean defect was -3.54dB.
936. Soans FP, Kahn SJ, Musch DC, Moroi SE. Thinner central corneas in eyes with more advanced glaucoma cuppinga new clue to glaucoma?
945. Bui CM, Joos KM. The effect of discontinuing nasal steroids on intraocular pressure in patients with glaucoma or ocular hypertension.
948. Tannenbaum DP, Nouri-Mahdavi K, et al. Performance of the OCT for discriminating early glaucoma from glaucoma suspects.
958. Chauhan BC, Artes PH, Hutchison DM, et al. Visual field and optic disc progression in glaucoma. The role of central corneal thickness.
2113. Barnebey HS, Pettigrew SC, Mallick S, et al. Three month comparison of the safety and efficacy of travoprost 0.004% timolol 0.5% ophthalmic solution to travatan and timolol 0.5%.
2129. Kogure S, Toda Y, Crabb D, et al. Does frequency doubling technology perimetry predict future scotoma with conventional automated static perimetry?
3305. Pratt AB, Medeiros FA, Bowd C, et al. Predicting early glaucomatous visual field loss using the Heidelberg Retina Tomograph.
3315. Kee C, Choul Yong P, Yun Taek K. Comparison of optic nerve head measurement by optical coherence tomography and confocal scanning laser ophthalmoscope.
3325. Krupsky S, Aloni E, Rachmiel R, et al. The diagnostic capabilities of the GDx with the VCC in detecting glaucomatous damage.
3333. Mueller-Holz M, Schmidt E, Boehm AG, Pillunat LE. Comparison of stereometric parameters of the optic nerve head using HRT and OCT.
3344. Quigley MG, Patel VR, Harasymowycz P. Determination of true optic disc area using a fundus camera technique: correlation with HRT measurements.
3413. Klein BEK, Klein R, Knudtson MD. Relationship of change in intraocular pressure to change in systemic blood pressure.
3472. Haymes SA, Artes PH, Hutchison DM, et al. Comparison of frequency doubling technology and standard automated perimetry for detecting glaucomatous visual field progression. A longitudinal prospective study.
4493. Hyman GF, Mehta JR. The association of central corneal thickness and ethnicity.
4494. Stodtmeister RP. Corneal pachymetry by optical coherence tomography and by ultrasound. A comparison.
4510. Blair DJ, Cantor L, WuDunn D, et al. Glaucoma and compliance: comparison of objective patient compliance information with respect to "QD" dosing versus "BID" dosing on patient medication compliance.
5543. Bujak MC, Yan DB. Correlation between cup-to-disc ratio asymmetry and optic disc size in glaucoma suspects and open angle glaucoma.

