
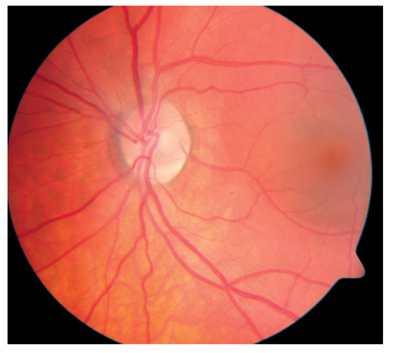
A: Choroidal neovascularization, either idiopathic or from histoplasmosis, can have a very similar appearance to idiopathic central serous chorioretinopathy (ICSC), says optometrist Jeffry Gerson, who practices in a retinal referral practice in Overland Park, Kan. So, its usually best to refer the patient for further evaluation to rule out CNV.
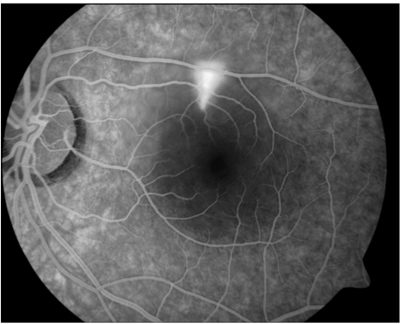
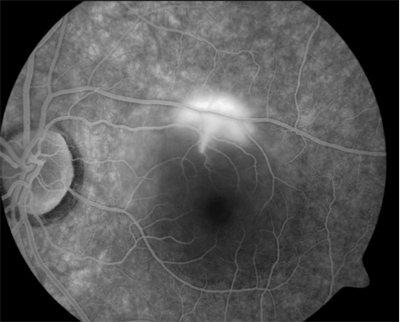
Patients with ICSC are typically young, male and have no other eye problems, Dr. Gerson says. When you suspect ICSC, as in this patients case, obtain both ocular coherence tomography and fluorescein angiography. The OCT will usually show neurosensory elevation and sometimes a serous retinal pigment epithelium detachment, he says. Fluorescein angiography will show the characteristic small area of hyperfluorescence that appears to mushroom in the late phase of the study.
Most patients with ICSC will not require any treatment, Dr. Gerson says. In fact, his practice does not treat patients at the initial visit. Once the diagnosis is confirmed by the above tests, we explain the condition to the patient and schedule another visit in approximately one month. It is not until then that we consider treatment, he says. At the one-month visit, the patient gets another OCT to monitor the amount of swelling.
 |
|
Before diagnosing idiopathic central serous chorioretinopathy, first rule out CNV. |
If the condition has not improved by the return visit and vision is still compromised, then provide patients with the treatment options. We know from previous studies that whether or not patients receive treatment, they tend to improve and have the same ultimate visual acuity.1,2 Patients who receive treatment tend to resolve more quickly, though, Dr. Gerson says.
The standard treatment is thermal laser, which ablates the vessel at the site of the leak seen on the angiogram. But if the leak is too close to the foveal center, then traditional treatment is not advisable because the scar will likely create a scotoma worse than the presenting symptoms, Dr. Gerson says. Usually in such a case, no treatment (except observation) is given. (However, new off-label treatments could be the answer. More on this below.)
In terms of comanagement, these patients often need only one or two visits to the retinal specialists office. If youre comfortable following the patient, you may only need the initial referral visit to confirm ICSC and rule out choroidal neovascularization, Dr. Gerson says. Often, the patient will remain in the care of the retinal specialist until the condition subsides, but once it does, you should expect the patient back in your office for long-term care, he says.
Q: I explained to the patient that he probably will not need treatment. But he is persistent and still wants to know whats available. Are there any new treatments on the horizon?
A: ICSC is a common condition, and the outcomes are usually good with either observation or thermal laser, Dr. Gerson says.1,2 However, patients with ICSC due to a subfoveal or juxtafoveal leak may need more advanced treatment. For these patients, investigators have tried several therapies. Intravitreal steroid injection has been tried, but without success.3 Indeed, systemic steroids appear to be a causative factor for ICSC.4 However, transpupillary thermotherapy (TTT) has shown significant success in patients who have chronic ICSC and/or foveal involvement.5,6
 |
 |
|
Fluorescein angiography demonstrates the characteristic small area of hyperfluorescence (left) that appears to mushroom in the late phase of the study (right). |
The exact reason for improvement is not yet known, Dr. Gerson says. One possibility: The decrease in choroidal blood flow causes enough decrease in flow to the retinal vessels to allow the leakage to stop. Whatever the reason, patients seem to do well. Two patients in Dr. Gersons practice participated in the above PDT study. Both have returned to 20/20 vision after one treatment and have not needed further therapy, he says.
1. Robertson DM, Ilstrup D. Direct, indirect, and sham laser photocoagulation in the management of central serous chorioretinopathy. Am J Ophthalmol 1983 Apr;95(4):457-66.
2. Burumcek E, Mudun A, Karacorlu S, Arslan MO. Laser photocoagulation for persistent central serous retinopathy: results of long-term follow-up. Ophthalmology 1997 Apr;104 (4):616-22.
3. Jonas JB, Kamppeter BA. Intravitreal triamcinolone acetonide and central serous chorioretinopathy. Br J Ophthalmol 2005 Mar;89(3):386-7.
4. Carvalho-Recchia CA, Yannuzzi LA, Negrao S, et al. Corticosteroids and central serous chorioretinopathy. Ophthalmology 2002 Oct;109(10):1834-7.
5. Wei SY, Yang CM. Transpupillary thermotherapy in the treatment of central serous chorioretinopathy. Ophthalmic Surg Lasers Imaging 2005 Sep-Oct;36(5):412-5.
6. Hussain N, Khanna R, Hussain A, Das T. Transpupillary thermotherapy for chronic central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol 2006 Jan 13:1-7.
7. Ober MD, Yannuzzi LA, Do DV, et al. Photodynamic therapy for focal retinal pigment epithelial leaks secondary to central serous chorioretinopathy. Ophthalmology 2005 Dec;112(12):2088-94.

