 |
Over the eight-year lifespan of this column, we have covered many topics related to binocularity. We have presented ways to enhance it with lenses and prism, ways to help recover it with vision therapy and a combination of the two. Even though we strive toward clear, single binocular vision, that is not always the best approach, nor is it even always possible to achieve.
In the February 2017 column, titled, “Binocularity, How Sacred Art Thou?” a case of diplopia was presented following surgical tumor removal and chemotherapy. After prism and 11 sessions of vision therapy failed to move the patient toward fusion, a spot patch was employed with great visual success and patient satisfaction. Later that year, in October, “Discretion is the Better Part of Valor” introduced a patient who had undergone decompression surgery for thyroid eye disease and developed subsequent noncomitant diplopia. In that case, a different approach—monovision in glasses—was discussed. Again, the flexibility to disregard the ingrained goal of binocular vision led to positive outcomes.
The following case is yet another outside-the-box approach to double vision for when your regular tools don’t make the cut.
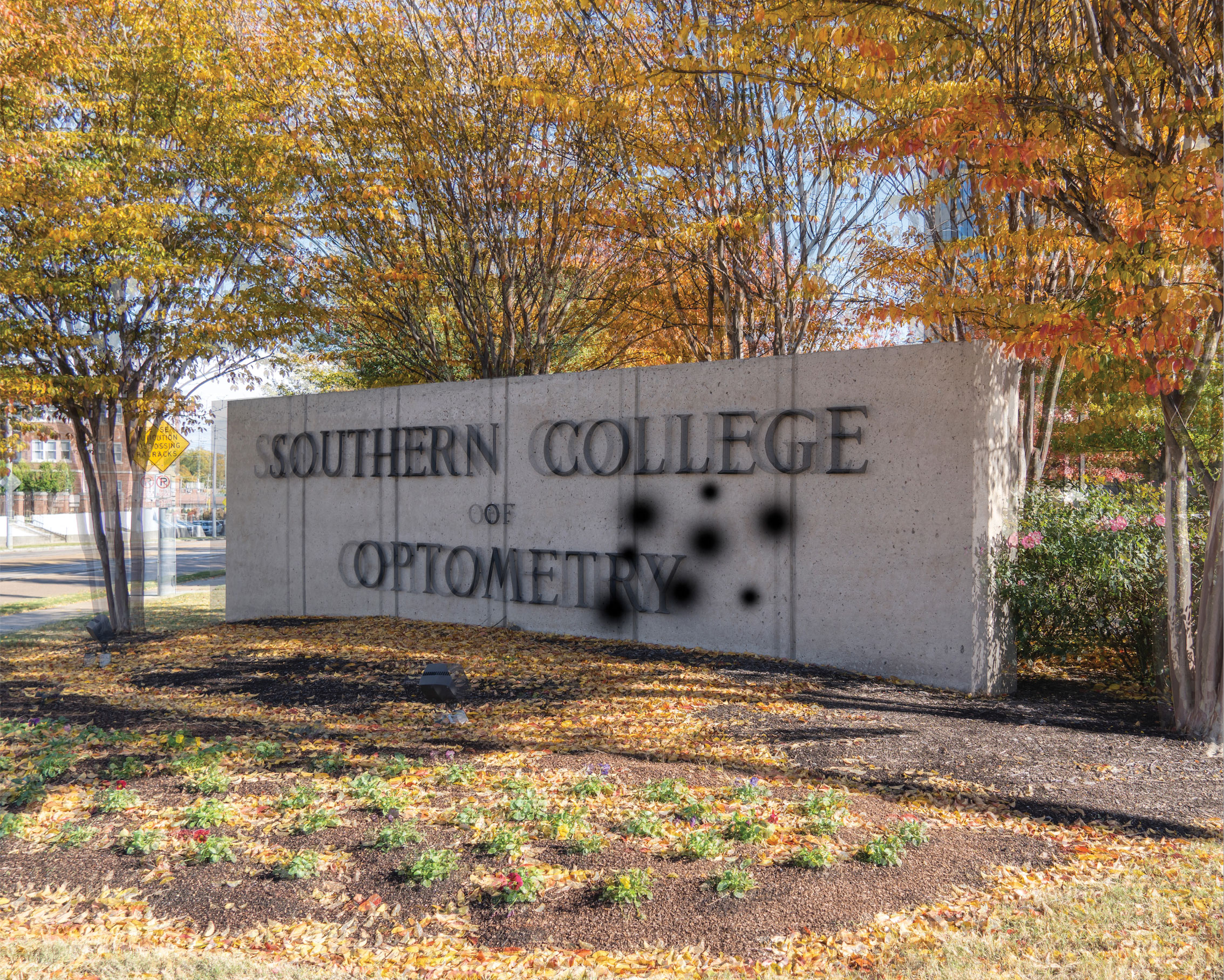 |
| An approximation of the patient’s vision based on her complaints. Photo: Phillip Tribble, Southern College of Optometry. Click image to enlarge. |
Case
A 56-year-old female presented with complaints of double vision and shadowing for the past three years following an acute angle closure in the left eye. She saw 30 images but had cataract surgery in the left eye, which reduced the number to six to seven images. She reported closing her left eye when reading and turning her head to reduce reflections when looking at screens. The left eye was her dominant eye. She was taking both Combigan (brimonidine/timolol, Allergan) and dorzolamide as prescribed by her glaucoma specialist. Her medical history was unremarkable.
The patient’s uncorrected acuity was 20/70 OD, 20/60 OS and 20/60+ OU. Corrected acuity was 20/20 OD and OU. No new glasses were prescribed post-cataract surgery, so no correction was present OS. Confrontation fields and ocular motility were normal. Cover test showed 3PD left hypertropia at distance and 6PD left hypertropia at near. The right pupil was normal to direct and indirect reaction, but the left was fixed at 4mm and was irregular in shape. Both pupils had a peripheral iridotomy, and the left had iris atrophy from three to six o’clock. The posterior capsule IOL was centered. The cornea showed stromal haze greater superior than inferior, which coalesced at three and nine o’clock. Pigment was scattered on the endothelium. The right cornea was unremarkable. The anterior chamber of the right eye was shallow, but the left was deep and quiet.
With a prescription of +4.00 -1.00x115 and -1.00 -0.50x055, her acuity was 20/20 and 20/30+2. Base-up prism of 1.5PD was shown in a trial frame, which reduced symptoms of doubling/shadowing but did not eliminate them altogether. The patient was prescribed two pairs of glasses, distance vision only and near vision only (+2.25 add) with prism in both, and was referred to the contact lens department for evaluation to assess whether her corneal issues might be causative of her symptoms. Corneal topography ruled out irregular astigmatism; it showed 45.8/4.7 @ 54.6 and 46.9/47.5 @ 87.8. The contact lens department chose to wait until the patient got her new glasses and showed adaptation to the prism as well as further reduction in symptoms before attempting a fit. She was scheduled for a follow-up a month after she began wearing her new glasses.
The patient returned with complaints of constant “splotchy” vision OS at both distance and near. She initially reported double vision but later described it as the light “expanding” in side gazes rather than obvious doubling. She disliked switching between her glasses, as she previously had progressive addition lenses. Her visual acuity was 20/15-1 OD, 20/40+1 OS and 20/15 OU at distance and 20/20 OD, 20/40 OS and 20/20 OU at near. Further exploration with prism proved unsuccessful.
At this point in the exam, our options were dwindling. Prism was off the table. Occlusion was discussed but rejected by the patient for cosmetic reasons. The dreaded black patch was not an option either. Bangerter foils, stick-on occlusion filters that blur the patient to specific acuity levels but are less cosmetically visible, were briefly considered. Still, given that her symptoms had been present for almost four years now, we needed something functional and cosmetically acceptable. How could we blur the left eye enough so that she might not notice the odd shadowing that she took issue with?
We pulled a +2.50 lens out of the lens kit and put it in front of her left eye while she was wearing her distance vision only glasses. The response was immediate and positive. The shadows were gone, and the patient’s body relaxed noticeably. To make sure this worked, we brought her into our 60-foot-long hallway and showed her again. Success, no shadows. We then showed her the +2.50 over the near vision-only glasses. Double success! Due to her dislike for the two-pair option, we reluctantly agreed to go back to the progression addition lenses for daily use and changed the left lens of the near vision-only pair for when she was going to read for a longer period of time. She was scheduled to return for follow-up in six weeks.
Upon returning, she was quick to say that she loved the progression addition lenses and could tolerate the near vision-only glasses in the morning while reading in bed, but once she used the progression addition lenses at any point during the day, she had trouble going back to the near vision-only glasses. In addition, the left eye was “fighting” in the near vision-only glasses but not in the progression addition lenses. She no longer noticed the shadows in the progression addition lenses but still did with the near vision-only glasses.
With a little trial and error, an extra +2.00 in front of the left eye eliminated the shadows, and there was no fighting. We changed the left eye of the near vision-only glasses up another +2.00 and asked the patient to return in another month. She was excited at the opportunity to read for pleasure again and left with a spring in her step.
Takeaways
The extra plus in the left eye blurred the input just enough to block the patient from acknowledging the shadows. As to why exactly she needed more plus in the near vision-only glasses than the progression addition lenses, we surmise that the variable prescription through which she was looking might have been helpful, or perhaps she was not looking directly in the right part of the lens in the first place.
This case highlights the intersection of medical and refractive care in optometry. Once the angle closure was addressed, the patient was unhappy with her vision. Not attending to her complaints and using every tool possible to improve her quality of life was simply not an option. As the medical side of our profession continues to expand, we cannot lose touch with the basic tenets of refractive care, sight and vision. With our help, this patient is finally regaining part of what was lost four years ago. You can and should do the same for your patients when given the opportunity.
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is an associate professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.

