Optometrists are well-acquainted with the two opposing muscles in the iris, the sphincter and the dilator, as we witness their effects daily in clinical practice. Pupil constriction (miosis) can either be stimulated by contraction of the iris sphincter or by relaxation of the iris dilator. On the other hand, pupil dilation (mydriasis) can either be stimulated by contraction of the iris dilator or by relaxation of the iris sphincter.
Miotic and mydriatic drops work by acting on these different muscles of the iris. The drops are able to control pupil size by targeting two parts of the autonomic nervous system: the sympathetic and parasympathetic systems. Let’s review their function and clinical role to better understand their present uses and why some of these agents are undergoing re-evaulation for potential new ones.
Behind the Scenes
The sympathetic pathway, mainly responsible for pupil mydriasis, involves a three-neuron pathway.1,2 The first neuron begins in the hypothalamus and descends through the midbrain to synapse onto a specific area of the spinal cord, known as the ciliospinal center of Budge. This synapse is located between the C8 and T2 vertebrae. The second neuron, which is the preganglionic neuron, exits the spinal cord, ascends through the thorax and synapses near the apex of the lung into the superior cervical ganglion. The third postganglionic neuron travels to the cavernous sinus and enters the orbit through the short and long ciliary nerves, synapsing to the iris dilator.1,2
Contrarily, the parasympathetic pathway is mainly responsible for pupil miosis.1,3 Pupil constriction starts when light enters the retina and activates the retinal ganglion cells—the beginning of the afferent arm—which then transmit their impulses into the optic nerve. This stimulus travels to the optic chiasm, through the optic tract and eventually reaches the pretectal nucleus. The impulses from the pretectal nucleus begin the efferent arm, which projects to the Edinger-Westphal nucleus. The Edinger-Westphal nucleus gives rise to preganglionic fibers, which then synapse with postganglionic neurons in the ciliary ganglion. Postganglionic neurons leave the ciliary ganglion to innervate the iris sphincter.1,3
 |
Tropicamide has a strong mydriatic effect. Click image to enlarge. |
Behind the Scenes
The sympathetic pathway, mainly responsible for pupil mydriasis, involves a three-neuron pathway.1,2 The first neuron begins in the hypothalamus and descends through the midbrain to synapse onto a specific area of the spinal cord, known as the ciliospinal center of Budge. This synapse is located between the C8 and T2 vertebrae. The second neuron, which is the preganglionic neuron, exits the spinal cord, ascends through the thorax and synapses near the apex of the lung into the superior cervical ganglion. The third postganglionic neuron travels to the cavernous sinus and enters the orbit through the short and long ciliary nerves, synapsing to the iris dilator.1,2
Contrarily, the parasympathetic pathway is mainly responsible for pupil miosis.1,3 Pupil constriction starts when light enters the retina and activates the retinal ganglion cells—the beginning of the afferent arm—which then transmit their impulses into the optic nerve. This stimulus travels to the optic chiasm, through the optic tract and eventually reaches the pretectal nucleus. The impulses from the pretectal nucleus begin the efferent arm, which projects to the Edinger-Westphal nucleus. The Edinger-Westphal nucleus gives rise to preganglionic fibers, which then synapse with postganglionic neurons in the ciliary ganglion. Postganglionic neurons leave the ciliary ganglion to innervate the iris sphincter.1,3
Mydriatic drops work by either inhibiting the parasympathetic pathway to the iris sphincter or by promoting the sympathetic pathway to the iris dilator. Drops that antagonize the parasympathetic pathway block acetylcholine, a neurotransmitter of the autonomic nervous system, from reaching muscarinic receptors, which are located within the iris sphincter.1,4 This leads to relaxation of the iris sphincter and promotes mydriasis.
On the other hand, mydriatic drops that promote the sympathetic pathway prevent the reuptake of norepinephrine, another neurotransmitter of the autonomic nervous system, from the synapse.1 This allows more norepinephrine to bind to alpha-one adrenergic receptors on the iris dilator, stimulating the activation of the iris dilator and leading to mydriasis.
Miotic drops work by either promoting the parasympathetic pathway to the iris sphincter or by inhibiting the sympathetic pathway to the iris dilator.1,5 Taking the former route, these drops mimic the activity of acetylcholine, and when they bind to muscarinic receptors, the iris sphincter contracts and pupil size decreases.
Drops that inhibit the sympathetic pathway can also stimulate pupil miosis. These drops selectively bind to alpha-two adrenergic receptors, which are responsible for decreasing the sympathetic tone. These receptors are located on the iris dilator, which when activated leads to a decrease in the amount of norepinephrine released into the synapse. This reduces the sympathetic tone on the iris dilator and encourages pupil miosis.
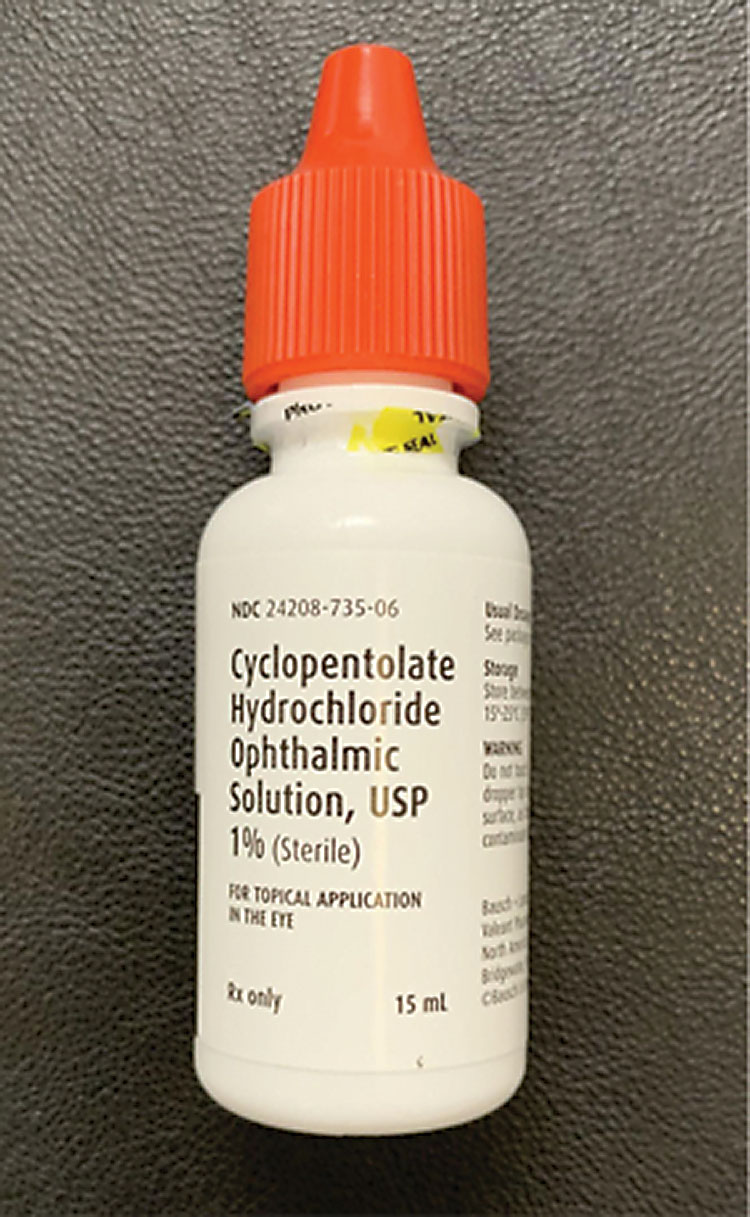 |
Cyclopentolate can effectively inhibit accommodation to help treat amblyopia and anterior uveitis. Click image to enlarge. |
Miotic Drops
These drops can be used for a number of things, including diagnosis of pupil abnormalities (e.g., Adie’s tonic pupil) and treatment of ocular hypertension, acute angle closure, dry eye and post-surgical glare.3 Exercise caution or avoid use altogether in patients who are pregnant, breastfeeding or at risk of retinal detachment. The following are several established drops and associated clinical pearls of each:
Parasympathomimetics. Pilocarpine is a miotic drop that is used primarily to treat ocular hypertension.6 It can effectively lower intraocular pressure (IOP) and is easily accessible. However, it can also induce myopic shifts and precipitate retinal detachments. For these reasons, pilocarpine is not commonly used in general practice.
Pilocarpine is a direct muscarinic acetylcholine agonist, or a parasympathomimetic. It binds to the M3 muscarinic receptor, an excitatory receptor in the iris sphincter and ciliary body. This leads to an upregulation of calcium and smooth muscle contraction of the iris sphincter and ciliary body. The contraction of the iris sphincter causes the pupil to decrease in size, and the contraction of the ciliary body opens the trabecular meshwork, decreasing IOP by enhancing aqueous outflow.
Sympathomimetics. Brimonidine and apraclonidine are miotic drops that are typically used to lower IOP and assist with post-surgical glare, ocular redness and diagnosis of pupil abnormalities (e.g., Horner’s syndrome).7 These drops are able to rapidly lower IOP and are readily available. They are contraindicated in patients with underlying asthma and those taking MAO inhibitors. They are also more strongly associated with allergic reactions.
Both of these drops exhibit selective alpha-two adrenergic agonist activity. They bind directly to alpha-two adrenergic receptors, which are inhibitory receptors of the sympathetic system. These receptors are present on the iris dilator, ciliary body and conjunctival blood vessels. They cause a downregulation of cAMP and a decrease in the sympathetic tone, leading to iris dilator relaxation, increasing uveoscleral outflow and decreasing aqueous production and vasoconstriction.
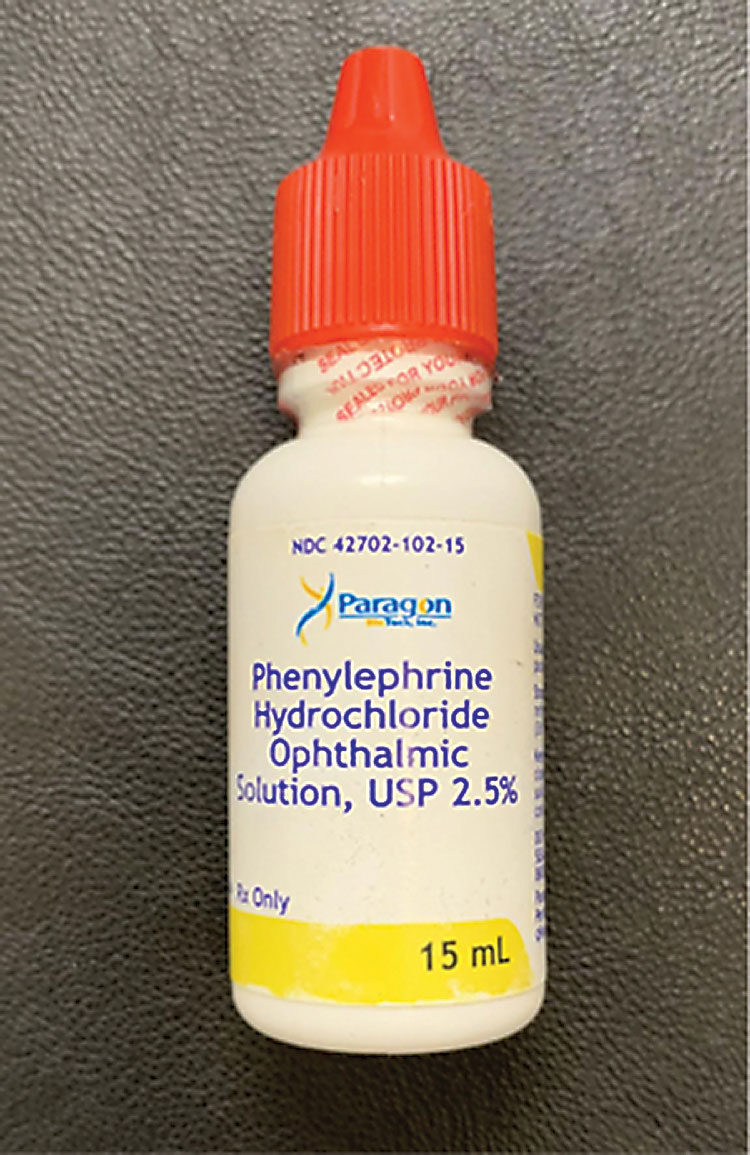 |
Phenylephrine should not be the sole drop used for dilated fundus examination, as it has a weaker mydriatic effect. Click image to enlarge. |
Mydriatic Drops
These drops can be used to perform dilated fundus examination, diagnose pupil abnormalities (e.g., Horner’s syndrome), treat anterior uveitis and engage in pharmacological penalization for amblyopia.2 Exercise caution or completely avoid use in patients who are pregnant or breastfeeding and in those who have anatomically narrow angles. The following are several established drops and associated clinical pearls of each:
Parasympatholytics. Tropicamide, cyclopentolate and atropine are all mydriatic drops that are traditionally used for dilated fundus examination, paralysis of accommodation, anterior uveitis treatment, myopia control and pharmacological penalization for amblyopia treatment.8-10
Tropicamide is typically used for dilated fundus exam, paralysis of accommodation and anterior uveitis treatment. It has a strong mydriatic effect, rapid onset and shorter duration of action in comparison with cyclopentolate and atropine. Its disadvantages include its ineffectiveness at inhibiting accommodation and its side effects of light sensitivity and blurred vision.
Cyclopentolate is commonly used to inhibit accommodation and treat amblyopia and anterior uveitis. It is effective at accommodation paralysis. On the other hand, it has a long onset of action, long duration of action and side effect profile that includes light sensitivity and blurred vision. The long duration of action makes this a viable drop of choice for anterior uveitis treatment to prevent anterior synechiae.
Similar to cyclopentolate, atropine is traditionally used to inhibit accommodation, manage amblyopia, treat anterior uveitis and provide myopia control. It has a strong mydriatic effect and is effective at inhibiting accommodation and slowing the progression of myopia. Its disadvantages mirror those of cyclopentolate.
The mechanism of action of each of these drops is identical: they all have direct antimuscarinic activity. They competitively bind to muscarinic receptors on the iris sphincter and ciliary body and inhibit their activity. This results in a downregulation of calcium and induces smooth muscle relaxation of the iris sphincter and ciliary body.
Sympathomimetics. Phenylephrine is a mydriatic drop that is traditionally used for dilated fundus examination, ocular redness relief and diagnosis of pupil abnormalities (e.g., Horner’s syndrome).11 It has a rapid onset of action and is easily accessible. However, it has a weak mydriatic effect and should not be used alone for dilated fundus examination.
Phenylephrine promotes the sympathetic pathway as a selective alpha-one adrenergic receptor agonist. Alpha-one receptors are excitatory receptors of the sympathetic system and reside in the iris dilator and conjunctival blood vessels. Activation of these receptors causes an upregulation of cAMP, which leads to iris dilator contraction and vasoconstriction.
Sympathomimetics and parasympatholytics. Paremyd (hydroxyamphetamine 1% and tropicamide 0.25%, Akorn) is a mydriatic that is traditionally used for dilated fundus examination.12 It has a rapid onset of action, reduced effect on accommodation and shorter duration of action. Its disadvantages include a reduced mydriatic effect on dark irides, decreased ability to inhibit accommodation and a side effect profile that includes light sensitivity and blurred vision.
Hydroxyamphetamine acts as an adrenergic agonist and blocks the breakdown of norepinephrine. This increases the sympathetic tone and indirectly initiates contraction of the iris dilator. Tropicamide has antimuscarinic activity and inhibits the muscarinic receptors on the iris sphincter, leading to pupil dilation.
In the Pipeline
The exploration of pharmaceutical advancements in the areas of myopia control, presbyopia and dilation is on the rise.Myopia. The increasing prevalence of myopia worldwide and its associated risk factors have led to a public health crisis. Historically, orthokeratology has been a leading option for slowing myopic progression, but ophthalmic drops are catching up and may potentially surpass this modality. Treatment with low-dose atropine has been increasing in popularity as more evidence continues to show its effectiveness. The Atropine for the Treatment of Myopia studies (ATOM 1 and ATOM 2) demonstrated the effectiveness of low-dose atropine. The investigators found that if the concentration of atropine is low enough, it is possible to avoid side effects of photophobia and blurred vision while still controlling myopic progression.13,14 The Low-Concentration Atropine for Myopia Progression (LAMP) study showed that 0.05% atropine had the most profound effect on minimizing myopic progression and axial elongation compared with 0.01% and 0.025%.15
Furthermore, new clinical studies are looking into the effectiveness of combination treatments for myopia control. The Bifocal and Atropine in Myopia (BAM) study is assessing the pharmacological effect of 0.01% atropine with the optical effect of soft bifocal contact lenses.16 Studies like these could lead to additional novel strategies to either optimize or provide greater slowing of myopia progression than single-treatment strategies.
 |
Paremyd is commonly the drop of choice for pupil dilation. Click image to enlarge. |
Presbyopia. Another area of focus for pharmaceutical companies has been developing noninvasive treatments for presbyopia. The race to develop effective treatments for the underlying cause of symptoms is underway.
One of the most interesting avenues of presbyopia treatment involves the use of topical drops to alter the pupil size to aid near vision. The challenge with miotic drops is avoiding too much pupil constriction, as this can have a negative impact on distance vision, night vision and even visual field. The key to a productive presbyopia drop is finding the miosis “sweet spot.”
Allergan is in the process of developing a presbyopic drop known as AGN-190584, which consists of an optimized formulation of pilocarpine, a muscarinic receptor agonist, the activation of which causes the iris sphincter and ciliary body to contract. This can enhance depth of focus and promote accommodation.17
Another company, Orasis, is also developing a miotic drop to constrict the pupil, known as CSF-1. Its complete composition has not yet been released, but it appears to be a combination of a parasympathomimetic agent and a nonsteroidal anti-inflammatory agent in an oil-based vehicle.18
In addition, Presbyopia Therapies is developing a presbyopic drop, called Liquid Vision, that produces miosis without stimulating accommodation. Rather than using pilocarpine, the active ingredient is aceclidine, which has a different mechanism of action that may provide a greater depth of field than pilocarpine.19
Visus Therapeutics is using a combination of ingredients to achieve a similar effect. Brimochol is a once-daily drop that combines carbachol and brimonidine tartrate to provide functional near vision for at least eight hours.20
While recent pharmaceutical strategies for presbyopia focus on altering pupil size and the ciliary body, others are investigating targeted approaches to alter the crystalline lens. Studies have suggested that the formation of disulfide bonds within the crystalline lens restricts the ability of the lens to change shape in response to ciliary muscle contraction.21 Due to its decline in flexibility with age, altering the lens shape could be a future avenue for novel treatment strategies.
Routine dilation. Newer mydriatic drops for routine dilation did not exist until recently. Eyenovia is nearing FDA approval for its new drop, MydCombi, which contains a fixed combination of phenylephrine and tropicamide. The drop would be the first microdosed ocular therapeutic that contains a smart delivery system. According to the company, Eyenovia’s Optejet dispenser is designed to provide a consistent, efficient and easy touchless application of two mydriatic medications. The bottle design of MydCombi contains no protruding parts, which can help prevent accidental interaction with the ocular surface.22
Reverse dilation. Currently, there are no FDA-approved drops to reverse pharmacological dilation. Ocuphire Pharma is currently developing an option that counteracts the side effects of routine pupil dilation. The drop, Nyxol (phentolamine 0.75%), is currently undergoing clinical trials to determine its safety and efficacy.
With a drop like this, subjects may be able to return to near baseline pupil diameter and accommodation within two hours, independent of the mydriatic agent used. Patients commonly defer routine dilation due to the long-lasting and disruptive side effects. If Nyxol shows promise, it could offer a novel solution to significantly improve the patient experience when it comes to routine dilation.23
Take-home Message
The autonomic nervous system plays an important role in managing pupil size. Parasympathetic and sympathetic innervation compete for control over the pupil. The sympathetic system dilates it, while the parasympathetic system constricts it. The diameter of the pupil at any time reflects the balance of these two forces acting simultaneously.The pupil response to miotic and mydriatic drops is directly dependent on which of these two autonomic systems is activated or inhibited. These drops continue to play a pivotal role in clinical practice, with new alternatives paving the way for treatments that were previously unavailable.
Dr. Asnaashari graduated from the UC Berkeley School of Optometry in 2018. He is a therapeutic- and glaucoma-certified optometrist in Sacramento, CA, and a Fellow of the American Academy of Optometry. One of his areas of expertise is specialty contact lenses. He has no financial interests to disclose.
| 1. McDougal DH, Gamlin PD. Autonomic control of the eye. Compr Physiol. 2015;5(1):439-73. 2. Lykstad J, Reddy V, Hannah A. Neuroanatomy, Pupillary Dilation Pathway. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 3. Belliveau AP, Somani AN, Dossani RH. Pupillary Light Reflex. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 4. Smith SV, Dake BA, Panneerselvam S. Pharmacologic dilation of pupil. EyeWiki. eyewiki.aao.org/Pharmacologic_dilation_of_pupil. December 29, 2020. Accessed March 17, 2021. 5. Harvey RD. Muscarinic receptor agonists and antagonists: effects on cardiovascular function. Handb Exp Pharmacol. 2012;(208):299-316. 6. Panarese V, Moshirfar M. Pilocarpine. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2020. 7. Yüksel N, Karabaş L, Altintaş O, et al. A comparison of the short-term hypotensive effects and side effects of unilateral brimonidine and apraclonidine in patients with elevated intraocular pressure. Ophthalmologica. 2002;216:45-9. 8. Alimgil ML, Erda N. The cycloplegic effect of atropine in comparison with the cyclopentolate-tropicamide-phenylephrine combination. Klin Monbl Augenheilkd. 1992;201(1):9-11. 9. Wallace DK, Repka MX, Lee KA, et al. Amblyopia preferred practice pattern. Ophthalmology. 2018;125(1):P105-42. 10. Li FF, Yam JC. Low-concentration atropine eye drops for myopia progression. Asia Pac J Ophthalmol (Phila). 2019;8(5):360-5. 11. Matsumoto S, Tsuru T, Araie M, et al. Pharmacokinetics of topical phenylephrine hydrochloride in the normal human eye. Jap J Ophthalmol. 1981;26(3):338-44. 12. Bartlett JD, Janus SD. Clinical Ocular Pharmacology. 5th edition. St. Louis, MO: Butterworth-Heinemann; 2008. 13. Chua WH, Balakrishnan V, Chan YH, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285-91. 14. Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (atropine for the treatment of myopia 2). Ophthalmology. 2012;119:347-54. 15. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2018;126(1):113-24. 16. Huang J, Mutti DO, Jones-Jordan LA, et al. Bifocal & atropine in myopia study: baseline data and methods. Optom Vis Sci. 2019;96(5):335-44. 17. Phase 3 efficacy study of AGN-190584 in participants with presbyopia. Allergan. www.allerganclinicaltrials.com/en/trial-details/?id=1883-301-013. Accessed March 23, 2021. 18. CSF-1 overview. Orasis. www.orasis-pharma.com/our-solution/csf-1-overview/. Accessed March 23, 2021. 19. Lipner M. A unique drop. EyeWorld. October 2014. www.eyeworld.org/article-a-unique-drop. Accessed March 23, 2021. 20. Visus Therapeutics announces FDA acceptance of IND to proceed with clinical development of presbyopia-correcting eye drop. Eyewire News. March 16, 2021. eyewire.news/articles/visus-therapeutics-announces-fda-acceptance-of-ind-for-presbyopia-correcting-eye-drop/. Accessed March 23, 2021. 21. Garner WH, Garner MH. Protein disulfide levels and lens elasticity modulation: applications for presbyopia. Invest Ophthalmol Vis Sci. 2016;57(6):2851-63. 22. Eyenovia announces FDA acceptance of the MydCombi NDA. Business Wire. March 2, 2021. www.businesswire.com/news/home/20210302005329/en/. Accessed March 23, 2021. 23. Ocuphire announces publication of MIRA-1 Phase 2b results demonstrating reduction of pharmacologically induced mydriasis by Nyxol. Eyewire News. March 5, 2021. eyewire.news/articles/ocuphire-announces-publication-of-mira-1-phase-2b-results-demonstrating-reduction-of-pharmacologically-induced-mydriasis-by-nyxol/. Accessed March 23, 2021. |

