Photodynamic therapy (PDT) remains a major area of study in the world of retinal subspecialists. Most of the papers presented at this years ARVO meeting are follow-ups of ongoing studies defining the success of PDT on various types of choroidal neovascularizaton (CNV). These include occult and juxtafoveal membranes, and PDT for other diseases, such as ocular histoplasmosis and pathological myopia.
Another area that continues to garner clinical interest: intravitreal triamcinolone acetonide (IVTA) injections. This corticosteroid appears to have an anti-angiogenic effect that stabilizes vision and reduces subretinal fluid when combined with photocoagulation or PDT.
Additionally, researchers presented studies on novel treatments for central retinal vein occlusion (CRVO) as well as new imaging technologies and surgical treatments for macular holes, such as internal limiting membrane peeling.
Photodynamic Therapy
A study group at the Bascom Palmer Eye Institute in Miami unveiled two-year results from a phase II clinical trial of Visudyne (verteporfin, Novartis Ophthalmics) therapy compared to a placebo for minimally classic subfoveal CNV.2273 Researchers divided 110 patients with CNV into three groups. One group received verteporfin therapy with reduced light fluence for 83 seconds. The second received verteporfin therapy with standard light fluence for 83 seconds, and the third received a placebo with a sham light treatment. Each verteporfin group was less likely to lose at least 15 letters of visual acuity when compared to the placebo group. The researchers advocate phase III trials.
Photodynamic therapy may lead to improved vision in AMD patients such as these.


Does verteporfin therapy on juxtafoveal lesions result in greater likelihood of vision improvement compared to subfoveal lesions? Researchers suspected this was the case when a few patients with juxtafoveal lesions showed dramatic improvement in visual acuity in two large-scale trials of photodynamic therapy. But now a Bascom Palmer Eye Institute study has cast doubt on this theory.3158 Investigators retrospectively looked at 31 eyes of 30 AMD patients who had juxtafoveal predominantly classic lesions and were treated with verteporfin therapy. Acuity improved by three lines in only 6% of patients, stabilized in 32% of patients and decreased by three lines in 19% of patients. These outcomes were similar to what would be expected for treatment of subfoveal lesions.
Verteporfin therapy also appears to be safe for treating subfoveal CNV secondary to ocular histoplasmosis syndrome. Corroborating its two-year findings, the Verteporfin in Ocular Histoplasmosis (VOH) study group found that in 15 patients who completed 48 months of follow-up, mean visual acuity was 69.5 letters at 24 months and 67.5 letters at 48 monthsan increase from baseline of 12.6 and 10.6 letters, respectively.2278 No patient experienced severe vision loss from baseline in this open-label, uncontrolled study.
Finally, pathological myopia that results in subfoveal CNV is another potential treatment target of PDT, according to a study team at the Eye University Clinic of Creteil in France.2277 Researchers extended a previous PDT study, enrolling 106 patients who had pathological myopia and adding two years of follow-up to their original one-year trial. Visual acuity remained stable, and no new safety concerns were noted. However, researchers cautioned that the results were not compared to placebo.
Triamcinolone Injections
Intravitreal injection of Kenalog (triamcinolone acetonide) in patients with CNV was another hot topic at this years ARVO meeting. Two papers suggested the injections helped stabilize visual acuity. A study at the Bascom Palmer Eye Institute in Miami found that 46 eyes that received PDT with intravitreal triamcinolone acetonide appeared to require fewer re-treatments than would be expected with PDT alone, and those treated did not suffer any adverse visual acuity outcomes.3159
A second study conducted by teams at Indiana University and the University of Wisconsin looked at 13 patients who had CNV and received the injections.3157 The researchers concluded the procedure was safe and at least the same as or better than PDT alone for stabilization of visual acuity and CNV leakage, caused by AMD or presumed ocular histoplasmosis syndrome.
Posterior sub-Tenons intravitreal injections of the drug also appear to stabilize visual acuity in patients with diabetic macular edema (DME), concludes a study team at the Cole Eye Institute in Cleveland.3464 Fifty patients with DME underwent the procedure and were followed up at one, three, six and 12 months. Visual acuities remained stable except at one month, when they showed a statistically significant improvement.

A Kenalog injection might be effective treatment for this patient with CNV.
Intravitreal triamcinolone for the treatment of vision loss secondary to macular edema from central retinal vein occlusion (CRVO) was evaluated by a study group at the Bascom Palmer Eye Institute.5238 In the 41 patients who underwent the treatment, 48% experienced a three-line improvement in visual acuity, but the median visual acuity of the group was unchanged from baseline. Recurrent macular edema and the need for re-treatment were common. Intraocular pressure spikes were also common, and one patient required glaucoma filtration surgery. Because this is the only known thromboxane treatment for macular edema secondary to CRVO, this study is seen as an important breakthrough.
Researchers at the WK Kellogg Eye Center and the University of Michigan evaluated intravitreal triamcinolone injections for the treatment of macular edema associated with retinal venous occlusive disease.4573 Of the 15 patients who underwent treatment, 66% showed three or more lines of visual acuity improvement. Of the remaining eyes, four were stable and one worsened. Again, seven eyes required additional treatment for IOP spikes.
In a University of Vienna paper, two groups of patients underwent injection of 4mg triamcinolone acetonide.5237 Each group had macular edema due to branch retinal vein occlusion (BRVO), and the other group had macular edema due to CRVO. Both groups experienced significant improvements in visual acuity, but the effect only lasted six months for the 12 CRVO patients and three months for the 10 BRVO patients. Six patients in the study required topical glaucoma medications for elevated IOP.
Other CNV Treatments
Several papers on other experimental treatments for CNV were presented. In one, anecortave acetate, a novel angiostatic cortisone, inhibited neovascularization in nine preclinical models of angiogenesis, according to study by the Vitreous-Retina-Macula Consultants of New York.1110 The drug is administered as a posterior juxtascleral depot with a specially designed cannula onto the outer surface of the sclera over the macula. Researchers found that a 15mm dose significantly reduced the amount of visual loss from baseline when compared with a placebo over 24 months. Investigators say they are planning a larger scale study to compare anecortave acetate to PDT.
The anti-VEGF monoclonal antibody Lucentits (ranibizumab, rhuFab V2) performed well in its phase I/II multicenter randomized trials. Researchers at Ophthalmic Consultants of Boston studied 64 patients with predominantly classic or minimally classic neovascular AMD.1109 Ranibizumab improved visual acuity at three- and six-month follow ups and was well tolerated. The most frequent adverse event was transient asymptomatic inflammation. No new anti-ranibizumab antibodies were detected in post-treatment.
In a paper presented by the C-PDT Study Group, baseline characteristics and rationale are discussed for a phase II trial of Celebrex (celecoxib, Pfizer) for treating the inflammatory response that sometimes occurs after PDT in patients with neovascular AMD.1186 This response appears to be mediated through the prostaglandin pathway. So, the use of celecoxib, a potent inhibitor of an enzyme in this pathway, could benefit PDT patients. Sixty patients were enrolled and divided into groups based on their predominant lesion type: predominantly classic, minimally classic and predominantly occult. This study is the first trial to access the ability of high-speed indocyanine green angiography to quantify changes in neovascular structures.
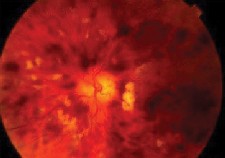
Ocular histoplasmosis is another potential treatment target for PDT.
Intravenous infusions of squalamine lactate improve visual acuity among patients with choroidal neovascularization in AMD, according to a multicenter study conducted by teams in Texas, Mexico, Pennsylvania and Louisiana.2362 Researchers looked at 40 patients between the ages of 51 and 92. Some 26% had three or more lines of visual acuity improvement, 74% retained their initial visual acuity or had less than three lines of loss at the four-month follow-up visit. In most patients, the treatment also inhibited new vessel formation without significant regression of existing lesions.
New Treatments for CRVO
Two studies concluded that retinal endovascular surgery (REVS) promotes visual recovery for CRVO patients, even more so when combined with intravitreal triamcinolone. REVS is a vitrectomy followed by cannulation of a branch retinal vein with injection of tissue plasminogen activator.
A multicenter study combined the experiences of four retinal surgeons who performed a total of 25 REVS procedures, nine of which also combined intravitreal triamcinolone.1051 Overall, 72% of patients recovered three or more lines of visual acuity, and 36% recovered eight lines or more. Though still significant, rates of visual acuity recovery were lower in eyes that did not receive intravitreal triamcinolone intraoperatively. The same conclusion was reached by a study group at the Retinal Association of South Florida, Margate, Fla.5226
Another new procedure, 25-gauge vitrectomyless limited sheath manipulation, showed impressive results in a retrospective study from the Doheny Retina Institute.4568 The treatment is meant for cases of branch retinal vein occlusion complicated by macular hemorrhage, macular ischemia and/or macular edema recalcitrant to grid laser photocoagulation. Of 16 eyes that underwent the surgery and were followed for at least 12 weeks, 94% experienced visual improvement, 81% experienced two or more lines of improvement, and 50% exhibited final acuity of 20/50 or better.
Imaging Technologies
The implantable miniature telescope is a prosthetic device designed to enlarge retinal images of the central visual field onto the central and peripheral retina. We are awaiting three-month safety and efficacy for patients who have stable, sight-depriving AMD in this multi-center, prospective clinical trial.2365
Optical coherence tomography (OCT) can be used to spot stage zero macular holes in the fellow eyes of patients with full-thickness macular holes, a Cambridge study concludes.Triamcinolone might stabilize vision in this patient with diabetic macular edema.1967 In 27 fellow eyes of 94 patients who have macular holes, OCT detected an abnormality of the vitreoretinal interface but normal foveal anatomy; the researchers describe this phenomenon as a stage zero macular hole. The study concluded that the presence of a stage zero macular hole was associated with a fourfold increase in the risk for bilateral macular hole formation.
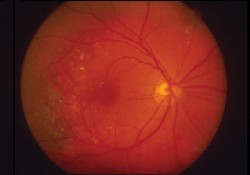
Triamcinolone might stabilize vision in this patient with diabetic macular edema.
Finally, a New York study group found that their ability to diagnose and measure diabetic macular edema was dramatically improved by using a Retinal Thickness Analyzer (RTA).4108
Treatment for Macular Holes
Internal limiting membrane (ILM) peeling and indocyanine green (ICG) staining do not appear to be harmful to patients when combined with pars plana vitrectomy, according to a New York study.1955 Eighty-three eyes undergoing macular hole repair were split into three groups: no ILM peeling, ILM peeling without ICG staining, and ILM peeling with ICG staining. All three groups were associated with good hole closure and improved visual outcome in most patients.
A Birmingham study found that pars plana vitrectomy for 26 eyes that had vitreomacular traction syndrome resulted in stable or improved vision for 84% of eyes.1993
1051. Bynoe LA, Hutchins RK, Lazarus HS, Friedberg MA. Retinal endovascular surgery for central retinal vein occlusion: initial experience of four surgeons.
1109. Heier JS. Review of Lucentis (ranibizumab, rhuFab V2) phase I/II trial results: six-month treatment of exudative AMD.
1110. Slakter JS.Anecortave Acetate in the treatment of age-related macular degeneration (AMD).
1186. Csaky KG, C-PDT Study Group. Phase II trial of Celebrex in photodynamic therapy (C-PDT) for neovascular age-related macular degeneration (AMD): rationale and baseline characteristics.
1955. Ahdoot M, Deramo VA, Fastenberg DM, et al. Visual outcomes after different surgical techniques in eyes undergoing macular hole repair.
1967. Chan A, Duker JS, Fujimoto JG. Stage zero macular holes: observations by optical coherence tomography.
1993. Mason JO, White MF Jr., Feist RM, et al. Long-term follow up of pars plana vitrectomy for vitreomacular traction syndrome.
2273. Rosenfeld PJ, VIM Study Group. Verteporfin in minimally classic CNV due to AMD (VIM)two-year results from a phase II controlled clinical trial.
2277. Soubrane G, VIP Study Group. Five-year results of verteporfin photodynamic therapy in pathologic myopia: third year of open label extension of the VIP Trial.
2278. Aaberg TM, VOH Study Group. Four-year results of verteporfin therapy for choroidal neovascularization (CNV) secondary to the ocular histoplasmosis syndrome (OHS): second year of an open label extension of the VOH Study.
2362. Garcia CA, Quiroz-Mercado H, Uwaydat S, et al. A phase I/II trial of intravenous squalamine lactate for treatment of choroidal neovasculariztion in age related macular degeneration (ARMD).
2365. Hudson HL, Martin DF, Berinstein DM, et al. The implantable miniature telescope in patients with macular degenerationresults of the Phase II/III IMT-002 trial at three months.
3157. Rogers DL, Danis RP, Gao H. Photodynamic therapy with verteporfin combined with intravitreal triamcinolone acetonide for the treatment of choroidal neovascularization.
3158. Barker DL, Puliafito CA. Rosenfeld PJ. Verteporfin therapy of juxtafoveal lesions in patients with neovascular AMD.
3159. Moshfeghi AA, Puliafito CA, Rosenfeld PJ. Verteporfin therapy with intravitreal triamcinolone in patients with neovascular AMD.
3464. Bakri SJ, Kaiser PK, Lerner LE. Twelve-month visual acuity outcomes after posterior sub-Tenon triamcinolone acetonide injections for diabetic macular edema.
4108. Weber PA, Soque J. The use of the Retina Thickness Analyzer (RTA) in evaluating patients with diabetic macular edema.
4568. Lakhanpal RR, Javaheri M, Barnes AC, et al. Vitrectomyless limited sheath manipulation using 25-guage instrumentation for complicated branch retinal vein occlusion.
4573. Mintz R, Johnson MW, Zacks DN. Intravitreal triamcinolone (Kenalog) injection for macular edema associated with retinal venous occlusive disease.
5226. Weiss JN, Bynoe LA. Retinal endovascular surgery, intravitreal triamcinolone and radical optic neurotomy for central vein occlusion.
5237. Krepler K, Sacu S, Ergun E, et al.The effect of intravitreal triamcinolone acetonide in patients with macular edema due to central or branch retinal vein occlusion.
5238. Lee JE, Mavrofrides EC, Smiddy WE, et al. Intravitreal triamcinolone for the treatment of macular edema from central retinal vein occlusion.

