When Technology Makes Us More Human
For some, Internet apps are improving connections with low vision patients.By Bill Kekevian, Senior Editor
When a 12-year-old Syrian refugee showed up to the Eye Institute at Salus University in Philadelphia, Erin Kenny, OD, had no way to communicate with her. The young girl spoke no English, was severely visually impaired and was accompanied by a teacher—from St. Lucy’s School for the Blind in Philadelphia—who spoke no Arabic. In previous encounters, Dr. Kenny communicated with a friend of the girl’s family who could translate, but he was unavailable at this visit.
“She was extremely introverted, didn’t make eye contact and was so shy,” Dr. Kenny reports. All she knew was the patient’s vision had clearly worsened. Dr. Kenny remembered a former colleague—a low vision specialist like herself—who had since moved to Canada and might be able to translate. She grabbed her iPad and reached out to Youssef Neema, OD, using Apple’s FaceTime application.
“You could just tell, the moment he started speaking Arabic, her [the patient’s] face lit up. He could look at her and she could look at him and they had a real conversation,” Dr. Kenny says. “So much can be lost in a language barrier.” The patient was so receptive, the girl’s teacher even asked Dr. Neema to make some inquires on her behalf. “There were things her teacher needed to know that she couldn’t ask her,” Dr. Kenny says.
After consulting with the patient, both doctors agreed she had extremely reduced central acuity and inferior visual fields, necessitating the use of a mobility cane. A lot of pediatric patients reject aids such as mobility canes for cosmetic reasons, but for refugees fleeing a war zone, cosmetic reasons may not be so trite. “She was uncomfortable with it because ISIS preys on those who seem weak,” Dr. Kenny explains.
 |
| Dr. Kenny uses apps in practice to help communicate with low vision patients. |
This isn’t the first time Dr. Kenny has turned to high-tech gadgetry for help in a complex situation. In another instance, a patient who was deaf presented with low vision, making communication a unique challenge. Without an aide to accompany the patient, “the exam won’t go anywhere,” she says. But when the patient turned to an iPad app to communicate with staff, Dr. Kenny was quickly able to identify the cause of his visual distress.
App to the Future
Dr. Kenny, who completed her low vision residency last summer, is among the many optometrists and other practitioners who are embracing the use of these so-called “smart” devices in the exam lane.1-3 In fact, she’s incorporated smartphone applications into her daily routine. “I have a list of apps that we’ve tried in our office that I give to patients at the end of each low vision exam,” Dr. Kenny explains. The list “breaks them down into categories—‘money reader’ apps and color identifiers, for instance—and I star the ones I like.”
Some apps are designed to step in for low vision aids, such as portable video magnifiers, which she says can help eliminate the stigma of living with low vision.
“Portable video magnifiers are amazing, but sometimes the costs are prohibitive for our patients. Smartphones can allow that magnification, the change in contrast and other things they need.”
Incorporating smartphone apps into regular practice has given low vision a “facelift,” says Dr. Kenny. “Our population is only going to get older, and the number of low vision patients is only going to increase.” These apps, she says, are helping bolster their quality of life.
|
1. Lewerenz D. The iPad as a low vision tool. Lecture presented at the AOA annual meeting, Philadelphia, June 28, 2014. Available at www.optometrysmeeting.org/documents/handouts/3115.pdf. Accessed January 11, 2017. 2. Wu R, Rossos P, Quan S, et al. An Evaluation of the Use of Smartphones to Communicate Between Clinicians: A Mixed-Methods Study. J Med Internet Res. 2011 Aug 29;13(3):e59. 3. Whitman L. Hospital clinicians’ iPad use: an interim report. Med Ref Serv Q. 2012;31(4):433-8.1. |
Post-concussion Vision Symptoms Can Keep Kids out of the Classroom
Students with concussion-related vision problems should undergo comprehensive vision assessments before returning to the classroom, new research suggests.
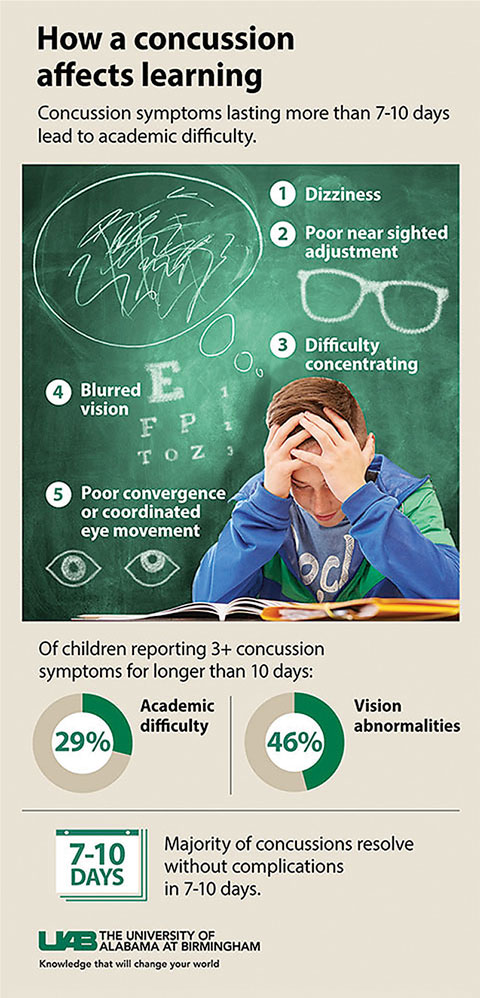 |
| Researchers created an infographic to help explain the effects a concussion can have on a child’s ability to return to the classroom. |
Although researchers recommend both ‘return-to-learn’ and ‘return-to-play’ protocols to evaluate concussion patients’ readiness to resume such tasks, less attention has been paid to the return-to-learn protocol than the return-to-play protocol—and patients with prolonged concussion symptoms report academic difficulties.1
“We focus so much on returning players to the field, but we lose focus on what happens to them the rest of the time,” says Marc Taub, OD, chief of vision therapy and rehabilitation at Southern College of Optometry.
Return-to-learn protocols rarely include vision evaluations in the decision-making process, despite evidence that suggests oculomotor tasks are affected in a majority of pediatric patients and convergence insufficiency yields higher total symptom scores.1
Researchers from the University of Alabama (UAB) at Birmingham set out to determine if a link exists between vision symptoms and reports of academic difficulty in pediatric patients suffering from prolonged post-concussive symptoms. Using data collected from Children’s of Alabama Concussion Clinic over a period of roughly seven years, researchers studied academic difficulties in a cohort of 276 children ages five to 18, who reported three or more concussion-related symptoms for 10 days or more, as well as a primary symptom of vision problems. Of these, 29% reported difficulties in school and 46% reported vision abnormalities, according to the study.2
Traumatic brain injuries impact near focus and eye movement coordination, leading to blurred vision and discomfort.2 “Because these problems are related to near vision, distance visual acuity testing conducted during a standard eye test may not show problems occurring with deskwork,” according to a press release.2
“Moving forward, physicians treating concussed patients should consider the damage done to the brain, specifically the vestibular and oculomotor functions, and how long this will affect a child’s progression and learning,” Mark W. Swanson, OD, lead author of the study, said in the press release.
While specific visual complaints and symptoms are acknowledged, Dr. Taub says, possible findings during a comprehensive vision evaluation and the most appropriate treatment options to enhance the ability to return to learn still need to be addressed further. “We see in the study population a correlation between concussion, visual symptoms and academic difficulty,” Dr. Taub says. “This study represents a step toward identifying the links between vision and learning.”
| 1. Swanson MW, Weise KK, Dreer LE, et al. Academic difficulty and vision symptoms in children with concussion. Optom and Vis Sci. 2017 Jan;94(1):60-7. 2. Rohan A. Vision symptoms following concussion can limit a child’s ability to return to the classroom. UAB News. Available at www.uab.edu/news/innovation/item/7864-vision-symptoms-following-concussion-can-limit-a-child-s-ability-to-return-to-the-classroom. Accessed 24 Jan 2017.1. |
CL Wear: Risky Business
A new survey may help identify risky behaviors that can lead to issues for contact lens (CL) wearers.1 The Contact Lens Risk Survey was developed to take a closer look at known and potential risk factors associated with soft CL wear among patients. It was also designed to determine differences in soft CL use for those with serious and significant conditions triggered by CL use, those with other red eye events not triggered by CLs and healthy control patients.
In the study’s results, patients with serious and significant conditions showed a higher propensity for risky behaviors compared with the other two groups, including overnight wear, internet purchasing, two-week replacement, failure to discard leftover solution on a daily basis and napping in lenses. The survey also introduced a new risk factor among patients with serious and significant conditions: sharing a bedroom. This was initially included in the survey because of reports that confined living situations potentially heighten disease transmission.2-4 The survey’s results instead suggested the opposite, possibly because not sharing a bedroom is different than living alone.
“We hope that in the future the survey will be used to help researchers and practitioners identify patients who are exhibiting risky behaviors associated with soft contact lenses,” says Heidi Wagner, OD, one of the study’s authors. “It would potentially be used to characterize the participant’s risk profile and provide individualized feedback regarding risky soft CL behaviors and assess interventions aimed at reducing soft CL-related complications.”
| 1. Sorbara L, Zimmerman AB, Mitchell GL, et al. Multicenter testing of a risk assessment survey for soft contact lens wearers with adverse events: a contact lens assessment in youth study. Eye & Contact Lens. October 13, 2016. [Epub ahead of print]. 2. Rimza EM, Kirk GM. Common medical problems of the college student. Pediatr Clin North Am. 2005;52:9-24. 3. Round A, Evans M, Salmon RL, et al. Public health management of an outbreak of group C meningococcal disease in university campus residents. Eur J Public Health. 2001;11:431-6. 4. Turner JC. How colleges can plan for the bird flu. Chronicle Rev. 2005;52:B20.1. |
Optometry’s Role in 21st Century Cures ActThe 21st Century Cures Act, a new law that aims to invigorate medical research and speed up the nation’s drug regulation system, includes $6.3 billion in new funding for research and alters the FDA approval process to hopefully make approvals smoother and quicker.While the impact will likely differ across medical fields, optometry played a part in shaping the act to ensure it makes sense for eye care. The American Optometric Association (AOA) “helped shape the bipartisan 21st Century Cures Act and prevent an irresponsible expansion of telehealth,” says Andrea P. Thau, OD, AOA president. Early proposals looked to expand telehealth service into Medicare, and one proposal even suggested new authority to replace face-to-face care. The AOA spoke out strongly against this, and it paid off. The final law simply calls for the Department of Health and Human Services to study possible effects of telehealth expansion. “From the very start, we made clear that, while we fully embrace appropriate uses of new and evolving technologies, we will do everything in our power to beat back those seeking to undermine the standard of care our patients need and deserve,” Dr. Thau says. “We were able to fight back and win against those seeking to downplay and discount the essential, in-person care provided by America’s doctors of optometry.” Bonamici S. H.R.34 - 21st Century Cures Act. Available at www.congress.gov/bill/114th-congress/house-bill/34/text. Accessed January 25, 2017. |
In the news
Lucentis (ranibizumab, Genentech) 0.5mg recently received FDA approval for the treatment of patients with myopic choroidal neovascularization (mCNV). Lucentis is the first FDA-approved anti-vascular endothelial growth factor (VEGF) therapy to treat mCNV in the United States—the fifth FDA-approved indication for Lucentis since its launch in 2006. A phase 3 study demonstrated treatment with Lucentis provided superior visual acuity gains in patients with mCNV compared with verteporfin photodynamic therapy.Researchers recently used confocal adaptive optics scanning light ophthalmoscopy to image individual retinal ganglion cells (RGCs) in an animal model. By collecting multiple images, varying in size and location, and combining them, they could visualize not just individual RGCs, but also structures within the cells, such as nuclei. Investigators hope this imaging modality may one day help assess glaucoma in humans before the retinal nerve fiber thins.
Ahad Mahootchi, MD, medical director at The Eye Clinic of Florida Same Day Surgery Center, recently performed the first pre-Descemet’s endothelial keratoplasty corneal transplant procedure with an eye bank-prepared Descemet’s membrane graft, delivered preloaded in the injector. The tissue, prepared by The Lions Eye Institute for Transplant & Research in Tampa, “made a very difficult surgery very easy. Having the tissue prestamped, prestained and preloaded in the injector saved me over an hour of time,” Dr. Mahootchi said in a news release.

