What is an optometrist to do when a patient has a condition that prevents you from examining the internal structures of the eye? We’ve all had patients with opaque corneas, dense cataracts or vitreous hemorrhages that completely or partially obscure our view of the posterior segment by conventional slit-lamp examination or biomicroscopy. In these cases, the best tool at our disposal is B-scan ultrasonography. Ultrasound has been used in eye care since the 1950s for accurately imaging the internal ocular structures when this information is not obtainable by other methods (Table 1).1
 |
| This patient is undergoing a transverse 3 o’clock scan. The patient looks nasally while the probe is placed at the 9 o’clock position with the probe marker oriented at 12 o’clock. |
It is capable of providing valuable information about the lens, vitreous, retina, choroid, sclera and orbit. B-scan ultrasonography is a painless, noninvasive method that can be performed easily in the clinic, or at a hospital bedside. It can be done safely on adults and children. It can also be a powerful diagnostic tool even when pathology is clinically visible (Table 1).
 |
| The top of this scan is the 12 o’clock position, the middle is the 3 o’clock position and the bottom is the 9 o’clock position. Click image to enlarge. |
Principles of Ultrasonography
B-scan ultrasound uses high frequency soundwaves that are transmitted from a probe/transducer into the eye. As these soundwaves strike the intraocular structures, an echo is reflected back to the probe and converted into an electrical signal. This signal is then reconstructed into a two-dimensional image on a monitor. The stronger the echo, the brighter the display. This process is repeated 1,000 times per second to produce a real-time display. The soundwaves used are inaudible to human ears because they have a frequency greater than 20KHz. Ophthalmic ultrasound most commonly uses a frequency of 10MHz. This allows for the best combination of tissue penetration and image resolution.
Another important aspect of all ultrasound instruments is the ability to adjust the amplification of echo signals. This is known as the gain control. The gain control is similar to the volume control on a radio. It changes the intensity of the returning echo displayed on the screen. It does not change the amount of energy emitted from the probe. A higher gain level allows for the capture of weaker echoes, such as those caused by vitreous opacities. A lower gain level will filter the weaker echoes, leaving only the strongest echoes, such as optic nerve drusen, the retina and the sclera. Lowering the gain effectively improves the resolution of the display, but in turn will also decrease the depth of the sound beam penetration.
| Table 1. Indications for B-Scan Ultrasonography | |
| When Direct Visualization is Impossible | When Ocular Structures are Visible |
| Lid abnormalities | Differentiating iris and ciliary body lesions |
| Corneal opacities | Ruling out ciliary body detachments |
| Hyphema/hypopyon | Differentiating intraocular tumors |
| Miosis | Differentiating serous vs. hemorrhagic choroidal detachments |
| Dense cataracts | Rhegamatogenous vs. exudative retinal detachments |
| Vitreous opacities | Differentiating disc drusen vs. disc edema |
Most ultrasound machines have the ability to use measurement calipers to assess lesion size, depth and distances within the eye. Some can zoom in and out, change image position, vary image contrast, save images as movies or pictures, use an A-scan cross vector overlay and generate final reports.
Getting to know all the features of your machine will enhance your ability to perform and interpret a B-scan properly.
Probe Orientations
The B-scan can be used in three different orientations for the eye: transversal, longitudinal and axial.
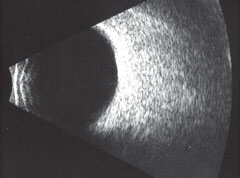 |
| This B-scan image portrays a normal, healthy eye. Click image to enlarge. |
In a transverse scan, the probe is oriented tangential to the limbus with the probe marker pointing superiorly for vertical scans and oblique scans, or nasally for horizontal scans. You designate the meridian being scanned by the clock hour in the center of the scan. A transverse scan is used to determine the lateral extent of a lesion.
In a longitudinal scan, the probe is oriented perpendicular to the limbus with the probe marker pointing to the center of the cornea. The scanned meridian is designated by the clock hour opposite of where the marker is placed. A longitudinal scan is used to determine the length (anterior to posterior) of the lesion, or to identify the insertion of membranes. The imaging of longitudinal scans always displays the anterior eye superiorly and the posterior eye inferiorly.
In an axial scan, the probe is placed on the center of the cornea with the patient looking straight ahead. Although this results in poor resolution of scans due to imaging through the dense media of the natural lens, axial scans are useful for locating lesions in the posterior pole and determining where lesions are in relation to anatomical markers such as the optic nerve and macula. Axial scans can be done horizontally, vertically or obliquely.
Basic Screening Examination Protocol
Here is how to perform a B-scan on a patient: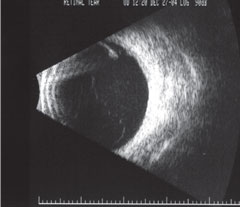 |
| B-scan of a retinal tear on high gain. Click image to enlarge. |
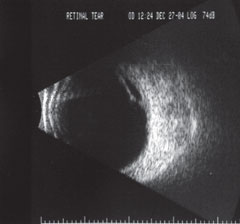 |
| B-scan of a retinal tear on low gain. Click image to enlarge. |
Step 1. Prior to beginning, make sure to disinfect the probe according to the manufacturer’s instructions.
Step 2. Begin by having the patient seated comfortably. The patient can be seated upright or reclined, with the head securely resting on the headrest.
Step 3. Instill one drop of topical anesthetic in each eye. This is especially important if you place the probe on the patient’s cornea or conjunctiva.
Step 4. Apply a coupling agent to the probe tip. Often, artificial tear gel or 2.5% methylcellulose are used; however, be sure to avoid using abdominal ultrasound gel, as it is considered an ocular irritant.
Step 5. Scan through the different meridians: transverse, longitudinal and axial, moving the probe tip from limbus to the conjunctiva. Make sure to observe the image on the screen while you are recording (Table 2).
Step 6. Save images as you go (For example, a tangential scan at 12 o’clock on the right eye can be saved as “OD-T12”). This will be beneficial when performing topographical evaluation of the images after completeing all the scans.
B-scan Pearls
Here are several tips on high quality scanning images:• Be sure to direct the patient’s gaze away from the probe and toward the meridian being scanned.
• The probe can either be placed on the patient’s closed eyelid or, for better resolution and certain globe position, place the probe directly on the conjunctiva.
• Remember that the top of the displayed image always correlates to the mark on the probe.
• Try to keep the probe perpendicular to the tissue being imaged, as doing so will improve resolution.
Table 2. Basic Screening Protocol Notes1. Transverse scans: Perform transverse scans of the 3, 6, 9, and 12 o’clock meridians. Maneuver the probe into the fornix to image more anterior regions.2. At minimum, perform longitudinal scans of 9 o’clock OD and/or 3 o’clock OS. These scans provide images of the macula. More meridians can be done if indicated. 3. Axial scans can be performed vertically or horizontally, or both. Axial scans are good for imaging the posterior pole. |
• Depending on what you are trying to image, developing a routine can be beneficial. For example, start with a tangential scan at 12 o’clock on the right eye, then perform a longitudinal scan at 12 o’clock on the right eye. Move clockwise through the meridians, alternating between transverse and longitudinal. Finish with vertical and horizontal axial scans. Then repeat the pattern on the left eye.
• The center of the scan offers the best resolution; try to center the area of interest in the scans.1
Topographic Evaluation
Topographic evaluation is performed once a lesion is found; this allows for detailed analysis regarding various aspects of the lesion. Typically, a standard sequence of steps is followed in this process. The transverse orientation is classically done first. The probe is placed on the opposite side of the globe as the lesion and moved from limbus to fornix. Following this pattern, sound beams gather information regarding the lateral extent of a lesion from posterior to anterior. Following this step, the lesion’s anterior to posterior extent is assessed using the longitudinal approach. Again, the probe is placed on the eye opposite the lesion; however, the marker is oriented toward the center of the cornea. Both of these scans together provide valuable information regarding the shape and dimensions of a lesion.
Axial scans may be performed to give a three-dimensional feel for the lesion. This additional approach is oriented to include both the lesion and the optic nerve in the same scan. Having multiple orientations is extremely valuable in the diagnosis and description of various ocular conditions. For example, by combining separate axial and transverse scans, a clinician can differentiate whether a funnel-shaped retinal detachment is open or closed.1It is also valuable to perform a simultaneous A-scan to gain additional topographical information of lesions such as a choroidal mass.
B-Scan Interpretation
Any review of B-scan ultrasound would be incomplete without discussing proper interpretation of the scan results. This brief review covers the most common findings in different ocular structures: |
| Above, the patient undergoes a transverse 3 o’clock scan. The patient looks nasally while the probe is placed at the 9 o’clock position with the probe marker oriented at 12 o’clock. |
• Vitreous. When examining the vitreous cavity on a B-scan, common conditions, such as a posterior vitreous detachment, can be evaluated and easily differentiated from more serious abnormalities such as a vitreous hemorrhage. In a young, healthy eye, the vitreous is mostly echolucent. When vitreous degeneration occurs, the cholesterol crystals within the liquefied vitreous will float and move within the vitreous cavity. On B-scan, these crystals will show as hyper-reflective foci within the vitreous cavity. If viewed dynamically, they will actually move as the eye moves. When a vitreous detachment occurs, the B-scan will show a reduced volume of the vitreous gel, with a clear delineation between the gel and liquid vitreous.
 |
| The top of this scan is the 12 o’clock position, the middle is the 3 o’clock position and the bottom is the 9 o’clock position. Click image to enlarge. |
Vitreous hemorrhage—a result of tearing due to conitions such as vitreoretinal traction, diabetic retinopathy and blunt trauma—will appear in a B-scan as low-intensity echoes within the vitreous cavity. This too will have movement with dynamic scanning. The echographic pattern of a vitreous hemorrhage will depend on its age and severity. Fresh mild hemorrhages appear as small dots or linear areas of low reflective mobile vitreous opacities, whereas in more severe older hemorrhages, blood organizes and forms membranes. Vitreous hemorrhages may also layer inferiorly, due to gravitational forces.
Asteroid hyalosis is a benign condition wherein calcium salts accumulate in the vitreous cavity. The calcium is relatively dense and produces multiple pinpoints, highly reflective vitreous opacities. Intraocular foreign bodies can be easily detected using ultrasound.
Ultrasound has the advantage of more precisely localizing the foreign object than other imaging modalities, such as CT or MRI. This can be extremely useful information for the surgeon removing the foreign body.
• Retina. When examining the retina on B-scan, conditions such as a retinal tear, retinal detachment and retinoschisis can be clearly differentiated. A retinal tear will appear on longitudinal scans as a “flap.” On occasion, the flap will still be connected to the posterior vitreous surface or membrane.
Subretinal fluid may form beneath the flap, elevating it further. A retinal detachment will show a highly reflective, undulating membrane (if viewed dynamically) on the B-scan. If it is a total retinal detachment, typically a funnel shape will be observed as the retina is still attached at the ora serrata and the optic nerve, typically. Retinoschisis, while difficult to differentiate from a retinal detachment on funduscopy, can be further evaluated using a B-scan. On B-scan, retinoschisis will appear dome-shaped, rigid and thin (it will not undulate like a retinal detachment if viewed dynamically).
 |
| The patient undergoes a longitudinal 9 o’clock scan. The patient looks temporally, the probe is placed opposite at 3 o’clock and the probe marker is pointed toward the 9 o’clock meridian. |
• Choroid. When viewing a B-scan, the choroid appears much thicker than the retina. This is true for normal eyes or when looking at conditions such as a choroidal detachment. A choroidal detachment will appear with a dome-shaped contour; larger detachments may consist of multiple domes that ‘kiss’ in the middle of the vitreous. Traumatic causes of choroidal detachments are often hemorrhagic, rather than serous. The subchoroidal space of a hemorrhagic detachment will show a host of dots, as opposed to a hollow area.
Differentiating between choroidal nevi and melanomas is another useful application for B-scan. Typically, melanomas arising from the choroid appear as smooth, dome-shaped lesions with low to medium internal reflectivity and a regular internal structures. Internal vascularity can also be detected. A classic collar button or mushroom-shaped lesion is evident in tumors that have broken through Bruch’s membrane. Occasionally, choroidal evacuation is seen at the base of the tumor, which represent the tumor invading further into the choroid. A melanoma can progress still further and extend through the scleral wall, known as extrascleral extension.
Disease Scans
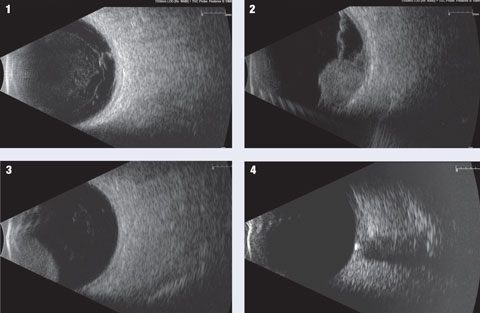
1. Posterior vitreous detachment with macular traction. 2. Choroidal melanoma with overlying retinal detachment. 3. Cilary body tumor. 4. Optic nerve drusen. Click image to enlarge. |
A choroidal nevus may appear to have a dome-shaped appearance as well; however, it differs from a melanoma in that it has high reflectivity and lacks internal vascularity.
Unfortunately, small melanomas may show an absence of low internal reflectivity and, therefore, may be difficult to differentiate from a small benign nevus.
Metastatic tumors have a much different echographic appearance. These tumors usually have an irregular, lumpy contour, an irregular internal structure, a medium-to-high internal reflectivity and little evidence of internal vascularity. Although exudative detachments occur with choroidal melanomas, similar-sized metastatic tumors typically have more extensive detachments. Extrascleral extension also can be seen with these tumors and is generally not helpful in the differentiation of the tumor.
• Ciliary Body. The ciliary body is visualized best with high-resolution scanning; however, a ciliary body detachment can extend into the peripheral choroid and can be seen on contact B-scan. A low-to-medium reflective cleft can be seen in the subciliary space. Ciliary body tumors are similar to those seen in the choroid and have similar echographic characteristics. Although most ciliary body tumors are melanomas, a variety of other tumors do arise in the ciliary body, including metastatic tumors, medulloepitheliomas and leiomyomas.
 |
| Software that accompanies ultrasound devices—such as the caliper tools being employed here—can measure any lesions discovered. Click image to enlarge. |
• Optic Nerve. Without interference of media opacities, the shape of the optic nerve, including the cup, is detectable with ultrasound. Differentiating the cause of a swollen optic nerve is a common clinical indication for B-scan. Papilledema, which is the result of increased intracranial pressure, will show a slightly widened optic nerve. With more elevated pressure, a black, empty-appearing area within the optic nerve sheath is apparent. This is known as a crescent sign and signifies the separation of sheath from optic nerve. Optic disc drusen, which can simulate papilledema, appear as highly reflective entities at the base of the optic nerve head.
Ultrasound can also be used to detect and differentiate optic nerve tumors, such as gliomas and meningiomas. An optic nerve glioma is a neoplasm that infiltrates the optic nerve parenchyma. On ultrasound, this is a smooth, fusiform mass with low-to-medium and regular internal reflectivity. An optic nerve sheath meningioma is a tumor of the optic nerve sheath. In contrast to a glioma, this tumor typically has a medium-to-high, irregular internal reflectivity with potential areas of calcification.
Know the Norm
It is vital to have a good grasp of what a normal ultrasound looks like. Not only are there minor differences in normal findings from patient to patient, but variation can exist within the same eye, due to the heterogenous nature of a normal eye. It is highly recommended that you gain as much experience as possible examining a normal eye to better evaluate patients with suspected eye disease. With increased experience, you will gain the confidence to evaluate a variety of ocular conditions.
As you become more experienced, you can expand your abilities to include more advanced techniques—such as examining the orbit and extraocular muscles. Your practice and, most importantly, your patients will benefit.
Dr. Urban is a staff optometrist at the Veterans Health Care System of the Ozarks in Fayetteville, AR.
Dr. Bunch is currently completing an optometry residency in ocular disease at the Veterans Health Care System of the Ozarks in Fayetteville, AR.
Dr. Ramey is currently completing an optometry residency in ocular disease at the Veterans Health Care System of the Ozarks in Fayetteville, AR.
Dr. Lighthizer is assistant dean for clinical care services, director of continuing education, and chief of both the specialty care clinic and the electrodiagnostics clinic at NSU Oklahoma College of Optometry.
| 1. Byrne SF, Green RL. Ultrasound of the eye and orbit, 2nd ed. Philadelphia, PA: Mosby, 2002:544. |