 |
After this complete evaluation, you conclusively diagnose the patient with POAG, and you are ready to initiate IOP-lowering therapy.
 |
|
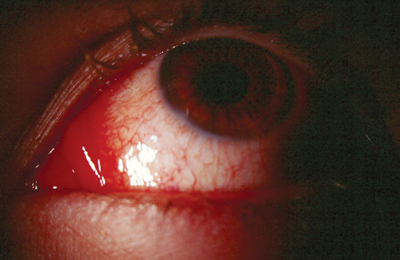
Hyperemia can lead to discontinuation or non-compliance of medication. |
But, suppose that, when the pa-tient returns, he is experiencing an unacceptable degree of conjunctival hyperemia? Or, the medication is well tolerated, but the IOP reduction is not clinically significant? Do you abandon this potent class of ocular hypotensive agents, or do you switch to another?
Some additional considerations:
How do you even decide with which prostaglandin to begin therapy?
Is there one that works better than the others?
Is there one with fewer side effects?
If one fails, will they all fail?
If adverse effects occur with one, will they occur with all?
These are the conundrums that make for this months column: how to sort out the prostaglandins.
Prostaglandin Overview
The prostaglandin medications are Xalatan (latanoprost, Pfizer), Travatan (travaprost, Alcon) and Lumigan (bimatoprost, Allergan). Prostaglandins are the most potent class of topical ocular hypotensive medications clinically available.1
These medications likely act by increasing aqueous outflow through the uveoscleral pathway and have been shown to surpass the pressure-lowering ability of topical beta-blockerslong held as the gold standard in glaucoma therapy.2-4
Many doctors initiate glaucoma treatment with one of the prostaglandins, and most have a personal favorite. Based on anecdotal experiences, practitioners may feel that one works better than the others or has a lower incidence of adverse effects.
However, to objectively sort out these medications, we must look beyond anecdotal experiences and concentrate on well-performed studies. We must also remember that IOP reduction is the most important consideration when prescribing prostaglandins and that ocular hyperemia is the most significant side effect that leads to discontinuation or non-compliance.
Prostaglandin Studies
The multi-center, randomized, masked, prospective Xalatan, Lumigan and Travatan (XLT) study, by Parrish and associates, simultaneously compared the effectiveness of these prostaglandins at reducing IOP and examined their adverse effects and patient tolerability.5
Patients who had either medically managed POAG or ocular hypertension had their medications discontinued for a period of time thought to be sufficient as to remove any residual effects of their medications. Then they were treated with one of the three prostaglandins in standard dosing.
Results showed that IOP was significantly reduced from baseline for all three medications, and the difference in the magnitude of the reduction was not statistically significant among the medications. This showed excellent efficacy of all of the medications. Furthermore, there was no significant difference among the medications in the persistence of pressure lowering or for the mean diurnal pressure throughout the study. This indicated that all three prostaglandins performed equally in their ability to reduce IOP, with equal persistence and stability of pressure reduction.
In terms of adverse effects, hyperemia was clearly the most commonly reported condition. There were fewer reported symptoms of hyperemia in the Xalatan-treated group. The intensity of the hyperemia was also less in the Xalatan group compared with the Travatan and Lumigan groups. Hyperemia was compared with standard photographs and objectively graded on an increasing scale of 0, 0.5, 1.0, 1.5, 2.0, 2.5, and 3.0. Although the Xalatan-treated group had less hyperemia, the mean hyperemia score of all three medications was less than Grade 1. All three medications were well tolerated ocularly and systemically.
Based on the XLT study, all three prostaglandins apparently make fine initial therapy choices. But what happens when the pressure reduction is less than desired or hyperemia is an issue? Does switching among the drugs make good therapeutic sense?
Switching among the Prostaglandins
One study revealed a reduction in IOP when patients who were unresponsive to Xalatan were switched to Lumigan.6 During this study, Xalatan non-responders experienced an additional mean IOP reduction of 3.5mm Hg with the use of Lumigan.
Another study revealed similar findings in POAG patients who had a statistically significant decrease in IOP when switching from Xalatan to Travatan.7 So, switching prostaglandins may be a good strategy when more pressure reduction is desired.
What about issues involving hyperemia? The hyperemic effects of prostaglandins are often directly related to the chemical structure of the drug used and may not occur with another prostaglandin.8,9 Given the dramatic effect of prostaglandins on IOP, when one prostaglandin causes side effects, it may be useful to try another one before changing the drug family.5,8,9
Prostaglandins are a significant class of medications that one should not prematurely abandon in the face of adverse effects or non-efficacy. All three are excellent medications that are well tolerated ocularly and systemically. Further, when faced with hyperemia or insufficient IOP reduction, trial of another prostaglandin may be a better choice than abandoning this important drug class altogether.
The bottom line: Dont give up too early and throw in the towel on prostaglandins. Always remember that there is an art, as well as a science, to treating patients who have glaucoma.
Drs. Sowka and Kabat are members of Alcons speakers alliance. They have no financial interest in any of the products mentioned.
1. Alexander CL, Miller SJ, Abel SR. Prostaglandin analog treatment of glaucoma and ocular hypertension. Ann Pharmacother 2002 Mar;36(3):504-11.
2. Toris CB, Camras CB, Yablonski ME, et al. Effects of exogenous prostaglandins on aqueous humor dynamics and blood-aqueous barrier function. Surv Ophthalmol 1997 Feb;41 Suppl 2:S69-75.
3. Netland PA, Landry T, Sulivan EK, et al. Travoprost compared with latanoprost and timolol in patients with open angle glaucoma or ocular hypertension. Am J Ophthalmol 2001 Oct;132(4): 472-84.
4. Sherwood M, Brandt J, for the Bimatoprost Study Groups 1 and 2. Six-month comparison of bimatoprost once-daily and twice-daily with timolol twice-daily in patients with elevated intraocular pressure. Surv Ophthalmol 2001 May;45 Suppl 4:S361-8.
5. Parrish RK, Palmberg P, Sheu W, XLT Study Group. A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: A 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmol 2003 May;135 (5):688-703.
6. Williams RD. Efficacy of bimatoprost in glaucoma and ocular hypertension unresponsive to latanoprost. Adv Ther 2002 Nov-Dec;19(6):275-81.
7. Hollo G, Vargha P, Kothy P. Influence of switching to travoprost on intraocular pressure of uncontrolled chronic open-angle glaucoma patients compliant to previously used topical medication. Curr Med Res Opin 2005 Dec;21(12):1943-8.
8. Nordmann JP. Medical treatments and practices. What should be done when a prostaglandin proves ineffective? J Fr Ophtalmol 2005 Jun;28 Spec No 2:41-4.
9. Feldman RM. Conjunctival hyperemia and the use of topical prostaglandins in glaucoma and ocular hypertension. J Ocul Pharmacol Ther 2003 Feb;19(1):23-35.

