 |
No optometrist wants to hear the words, “A pencil hit my eye, and now I am in so much pain.” However, everyday accidents do occur, and we have to be prepared when they walk in the door.
Case History
A 15-year-old boy was sent to the school nurse after being struck in the left eye by a pencil that was thrown from across the classroom. The boy immediately noted pain, blurred vision and excessive tearing. After being evaluated by the school nurse, he returned to class and finished the school day with only mild irritation in the left eye. Upon waking the next morning, he noted more irritation and worsening of his vision. After a few hours at school, he was sent to the school nurse again for redness and irritation. He was then referred to a local optometrist for evaluation.
 |
|
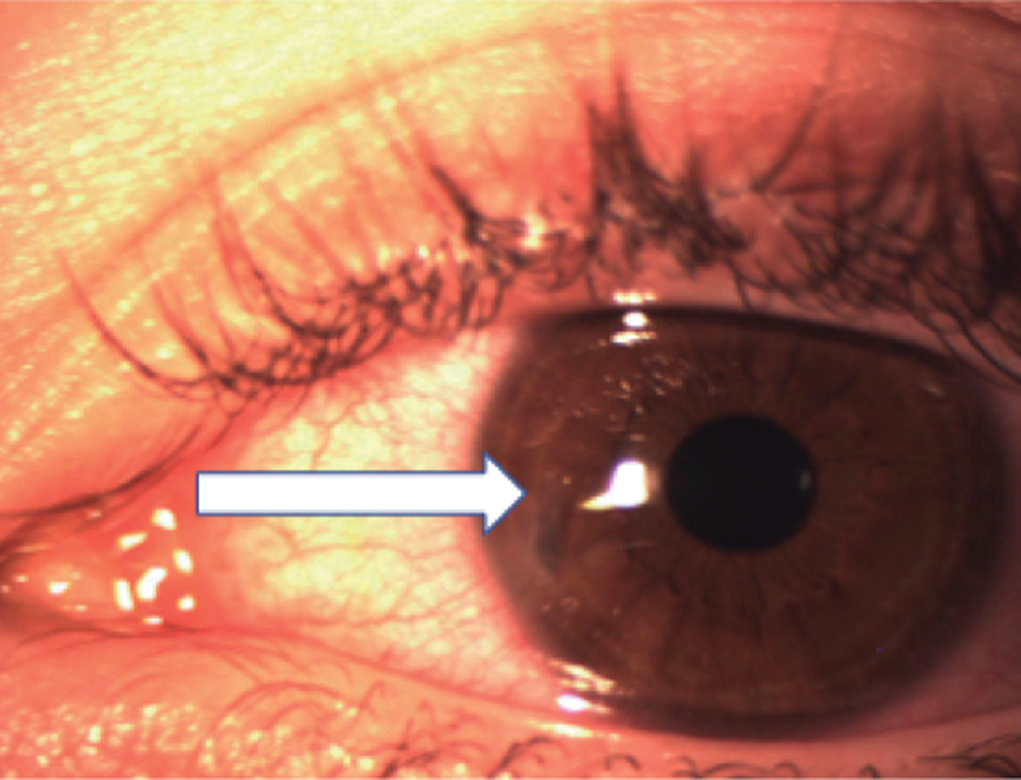
This patient was diagnosed with an open globe injury. Click image to enlarge. |
Examination
His vision was 20/200 OS with an intraocular pressure of 3mm Hg and a shallow anterior chamber. The pupil was regular and round, without peaking. There were 2+ cells in the anterior chamber and mild flare. He had a small round, full thickness corneal defect, which was Seidel-positive. An eye shield was then placed over the eye, and he was referred to our clinic.
We were in agreement with the patient’s local optometrist, who diagnosed him with an open globe injury secondary to corneal perforation. We placed the patient on topical moxifloxacin, oral Levaquin (levofloxacin, Johnson & Johnson) due to the amount of time that had passed since the accident and a cycloplegic for the pain. We used timolol—an aqueous suppressant—and a bandage contact lens with the hopes the wound would self-seal.
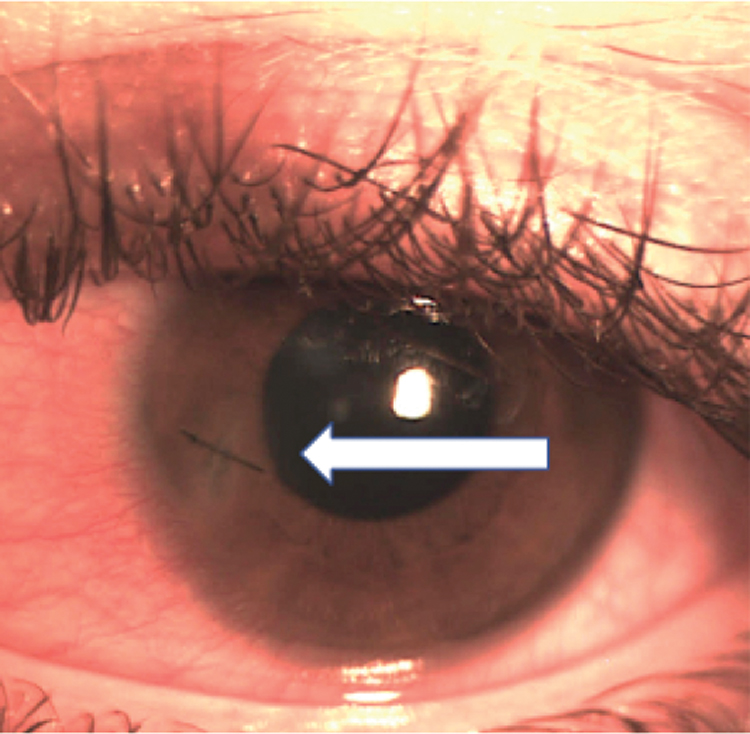
When the boy returned the next day, the wound was still leaking; therefore, surgical intervention was warranted. One suture was strategically placed to close the wound, and the patient was injected with intracameral moxifloxacin and started on topical steroids. When the patient returned the day after surgery, the vision in his left eye was 20/20, his intraocular pressure was 12mm Hg and he was Seidel-negative. He then began his post-op steroid taper.
Discussion
The incidence of open globe injuries in the United States is 3.4 per 100,000 people each year, with the vast majority occurring in patients between the ages of 17 and 29 years old and in men.1 Often the first doctors to see these patients after an injury, ODs should perform a thorough case history, pupil, visual acuity, intraocular pressure and slit lamp assessment. Do not check intraocular pressure with Goldmann tonometry if you suspect a full-thickness laceration.
 |
|
A strategically placed suture can help close a leaking wound. Click image to enlarge. |
Signs of open globe injury include penetrating lid injury, bullous subconjunctival hemorrhage, shallow anterior chamber, blood in the anterior chamber, peaked pupil, iris disinsertion, lens dislocation, vitreous hemorrhage or retinal detachment and loss of red reflex.
It is important to rule out the presence of an intraocular foreign body with imaging. A CT scan of the brain and orbits is considered standard of care if you suspect an intraocular foreign body. A B-scan can also be performed but requires extreme caution to make sure minimal pressure is applied to the eye.
After diagnosing a patient with a ruptured globe, immediately refer them to an ophthalmologist for surgical repair. Open globe injuries should be treated within 12 to 24 hours to decrease endophthalmitis risk.2 An eye shield should be applied and the patient instructed to not consume any food or drinks in case they have to be placed under general anesthesia during surgical repair. If broad-spectrum antibiotics are available, give a dose until they meet with an ophthalmologist.
Treatment
The ophthalmologist will determine the treatment plan. However, optometrists hold an important role in diagnosing and comanaging these patients. A conservative approach for wound leaks may include bandage contact lenses, aqueous suppressants or corneal glue. These therapies allow the cornea to heal itself without surgical repair. If the wound continues to leak, like it did in this case, surgical repair will probably be necessary.
After surgery, the patient may then be placed on a topical steroid to reduce inflammation. Regardless of which approach is used, the patient will be placed on broad-spectrum oral antibiotics, topical antibiotics and sometimes intracameral or intravitreal antibiotics to prophylactically avoid endophthalmitis.3 The addition of a topical cycloplegic can help with patient comfort. If the patient is unsure about their immunization history, administer a tetanus shot. Monitor these patients closely, with follow-up visits each day to ensure infection doesn’t occur.
The Ocular Trauma Score
This is used to educate, set expectations and prepare patients and their families following an open globe injury. Visual acuity has remained one of the strongest predictors of the outcome.4 Combining the patient’s entering visual acuity and additional risk factors reveals the estimated percentages of different visual prognoses. Our patient had a 44% chance of seeing better than 20/40. Thankfully, the odds were in his favor, and he was able to see 20/20 again.
Dr. Zimprich is a residency-trained optometrist at Vance Thompson Vision in Sioux Falls, SD. She specializes in anterior segment surgical care, including cataracts, corneal diseases, glaucoma and refractive surgeries.
1. Batur M, Seven E, Esmer O, et al. Epidemiology of adult open globe injury. J Craniofac Surg. 2016;27(7):1636-41. 2. Blanch RJ, Bishop J, Javidi H, et al. Effect of time to primary repair on final visual outcome after open globe injury. Br J Ophthalmol. 2019;103(10):1491-4. 3. Wajda B. The Wills Eye Manual. Philadelphia: Lippincott Williams & Wilkins; 2016. 4. Scott R. The Ocular Trauma Score. Community Eye Health. 2015;28(91):44-5. |

