A 72-year-old white male presented with a sudden onset of decreased vision in his right eye. He said the vision loss was painless and was unchanged since its onset a week earlier.

This patient had a longstanding history of decreased vision in his left eye, due to two separate incidences of branch retinal vein occlusion with associated macular edema and retinal neovascularization. He subsequently underwent macular grid laser and panretinal photocoagulation. The patient, who was diabetic, also had mild non-proliferative diabetic retinopathy in both eyes.
Besides diabetes mellitus, which he controlled with insulin, the patients medical history was significant for pituitary microadenoma, hypertension, hyperlipidemia and coronary artery disease. The patient also had undergone coronary artery bypass surgery and was diagnosed with congestive heart failure. A recent MRI showed that the microadenoma was stable.
The patients medications were as follows: atenolol for his hypertension, simvastatin for his hyperlipidemia, furosemide and isosorbide for his coronary artery disease, and digoxin for the congestive heart failure. He also used a potassium supplement and took 325mg of aspirin daily as anti-coagulation therapy.
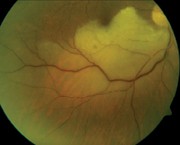
1. Fundus photo of the right eye at initial presentation. Note the changes in the blood vessels inferiorly.
Best-corrected central visual acuity, measured with a Feinbloom chart, was 5/60 at 5 feet in both eyes. Extraocular motility was full in both eyes. Confrontation fields revealed an absolute superior visual field defect in the right eye and were full to careful finger counting in the left. Pupils were equal and round without afferent pupillary defect.
The anterior segment examination was unremarkable and revealed no iris neovascularization in either eye. Intraocular pressure was within normal limits in both eyes. The lenses showed 1+ nuclear sclerosis in both eyes.
Dilated fundus examination revealed optic nerves with normal cups and distinct margins. The right optic nerve showed moderate inferior temporal pallor. The left nerve was normal. Other changes can be seen in the photos (figures 1 and 2).
Take the Retina Quiz
1. What is the correct diagnosis for the patients right eye?
a. Myelinated nerve fiber layer.
b. Active Toxoplasma retinitis.
c. Branch retinal artery occlusion.
d. Commotio retinae.
2. What is the most likely etiology of this finding?
a. Atherosclerosis of the retinal vasculature.
b. Infestation by an obligate intracellular protozoan.
c. Trauma.
d. Embolic event.
3. What can we observe in the inferior temporal retinal arteriole of the patients right eye?
a. Sausaging phenomenon.
b. String of fibrinoplatelet emboli.
c. Segmentation of the blood column.
d. Early sclerosing of the retinal arteriole.
4. What further medical testing is likely warranted for this patient?
a. Blood pressure measurement.
b. Carotid ultrasound.
c. Echocardiogram.
d. All of the above.
5. Which treatment is beneficial, provided the patient presents within 24 hours of onset of vision loss?
a. Ocular massage.
b. Pharmacologic lowering of intraocular pressure.
c. Anterior chamber paracentesis.
d. None of the above.
For answers, click here.
Discussion

2. Fundus photo of the left eye, which has a history of two prior branch retinal vein occlusions. Note the collaterals temporal to the macula as well as peripheral scatter laser scars.
This patient had a branch retinal artery occlusion (BRAO) in his right eye. Because he did not present until one week after the onset of vision loss, nothing could be done to reverse the effects of the BRAO. Even if he had presented within 24 hours of onset, the prognosis for visual recovery would have remained poor. Non-invasive procedures such as ocular massage, pharmacologic lowering of IOP or minimally invasive techniques such as anterior chamber paracentesis have not been proven to be effective at reversing the natural course of the disease.
Reports of successful treatments for central retinal artery occlusion (CRAO) and BRAO are anecdotal. In one study, a 77-year-old woman with a CRAO underwent successful neodymium:YAG laser arteriotomy with embolectomy approximately four hours after the onset of her symptoms.1 In another, an 82-year-old woman with an acute BRAO and a visible retinal arterial embolus underwent successful treatment with an intravenous injection of prostaglandin E1, a potent vasodilator.2
While these reports hold interesting possibilities for retinal artery occlusions reported promptly, no definitive treatment has proven to reverse the natural course of the disease.3 Still, systemic implications become extremely important to consider when a patient presents with retinal artery occlusion.
Our patients blood pressure that day measured 144/80. We referred the patient for ultrasound (pulsed duplex and color Doppler) of the carotid and vertebral arteries, which we believed were the most likely source of the ocular emboli. The radiologist reported no hemodynamically significant stenosis of either side. Had there been a significant amount of carotid artery stenosis, carotid endarterectomy may have been indicated.
Our patient had previously been followed for paroxysmal atrial fibrillation and moderate left ventricular dysfunction, so an echocardiogram was warranted. He also underwent transesophageal echocardiogram, which revealed no obvious cardiac source of embolism. Although there was no obvious source of embolization, we discussed increased anticoagulative therapy with the patients primary-care physician. The PCP prescribed Plavix (clopidogrel bisulfate, Bristol-Meyers Squibb).
One month later, visual acuity O.D. improved to 20/200. We referred him to the low vision clinic, where he received various low vision aids for reading.
This case was written by David N. Lynne, O.D., a resident at the Veterans Affairs Medical Center in Huntington, W.Va.
1. Reynard M, Hanscom TA. Neodymium:yttrium-aluminum-garnet laser arteriotomy with embolectomy for central retinal artery occlusion. Am J Ophthalmol 2004 Jan; 137(1):196-8.
2. Steigerwalt RD Jr, Pescosolido N, Corsi M, et al. Acute branch retinal arterial embolism successfully treated with intravenous prostaglandin E1case reports. Angiology 2003 Jul-Aug; 54(4):491-3.
3. Mueller AJ, Neubauer AS, Schaller U, et al. Evaluation of minimally invasive therapies and rationale for a prospective randomized trial to evaluate selective intra-arterial lysis for clinically complete central retinal artery occlusion. Arch Ophthalmol 2003 Oct;121(10):1377-81.

