 |
Because a majority of patients with dry eye have the evaporative form that accompanies meibomian gland dysfunction (MGD), with or without aqueous deficiency, researchers, manufacturers and clinicians have all focused on methods to clear obstructed meibomian glands and restore the flow of healthy lipids into the tear film.1 This has led to the rise of many in-office treatments that provide the promise of symptomatic relief for patients with MGD, as well as new revenue opportunities for clinicians and practices.
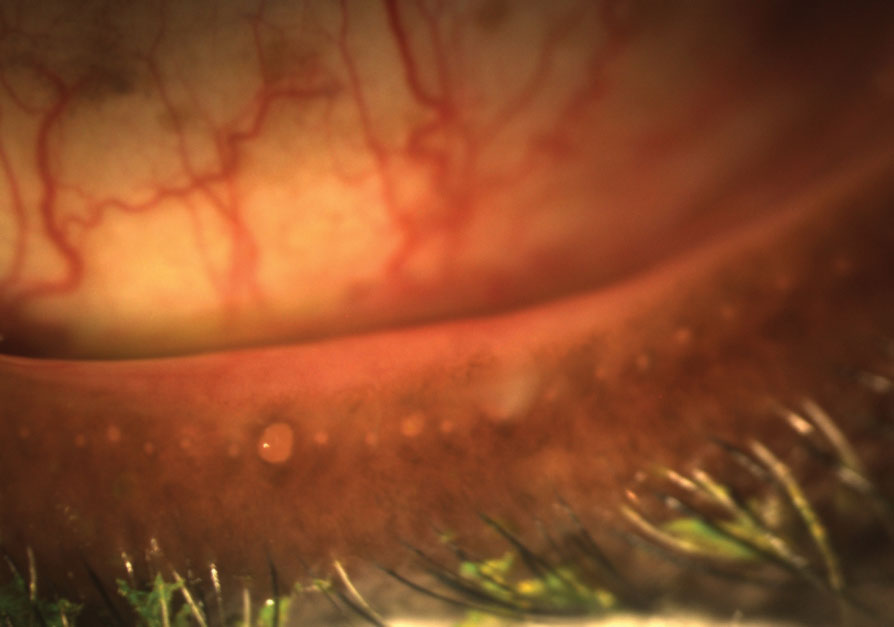 |
| These obstructed meibomian glands respond to digital pressure by releasing thickened, cloudy meibum. Newer treatments seek to improve results and patient comfort. Photo: Doan Huynh Kwak, OD |
Tried and True
The most established treatment for MGD is Lipiflow (Johnson & Johnson Vision), which has many peer-reviewed papers in the literature to support its efficacy. The 12-minute, automated treatment heats the inner eyelid closest to the meibomian glands and simultaneously massages the lids to evacuate gland contents. Several studies have reported sustained effects over 12 months or more following a single treatment, including significant reductions in symptoms and improvements in MG secretions.2-4 Reports also note increased comfortable contact lens wear time of more than four hours following a single Lipiflow treatment.5
Adjunctive Therapies
A number of other in-office strategies can help to increase the efficacy of home-based lid hygiene measures and extend the effectiveness of therapeutic treatments:
Lid debridement. Mechanical debridement/scaling of the line of Marx and the lid margin removes keratin from the meibomian gland orifices that can obstruct lipid expression to the ocular surface; these keratin deposits can also predispose the patient to blepharitis. One study found that debridement on its own provided statistically significant symptom relief and improved meibomian gland function.6 The technique can have a synergistic effect when combined with other treatments that heat or express the glands.
Blephex. According to the dry eye blepharitis syndrome (DEBS) theory, mechanical removal of biofilm may have a significant impact on dry eye disease, supporting therapeutic interventions such as Blephex.7 More than just a simple debridement, this procedure removes biofilm contributing to MGD and DEBS from the meibomian glands, lid margins and lashes. A spinning, disposable, medical-grade micro-sponge removes scurf and debris, exfoliating the affected areas. The brush cleans all four lids in seven to 10 minutes.
Intense pulsed light (IPL). Dermatologists have used these systems for years to treat acne rosacea. Treatments are performed with 500nm to 1,200nm light pulses for 20 to 30 minutes, and can be repeated every four to five weeks. Doctors with aesthetic practices noticed that treatment often seemed to improve dry eye symptoms as well, and some began performing IPL for MGD. The theory is that high-intensity light is absorbed by oxyhemoglobin, potentially reducing the amount of inflammatory mediators reaching the meibomian glands. Although preliminary results have shown some improvement in tear break-up time (TBUT) with IPL, it is not entirely clear which patients benefit most and whether IPL should be considered a primary or adjunctive treatment.8
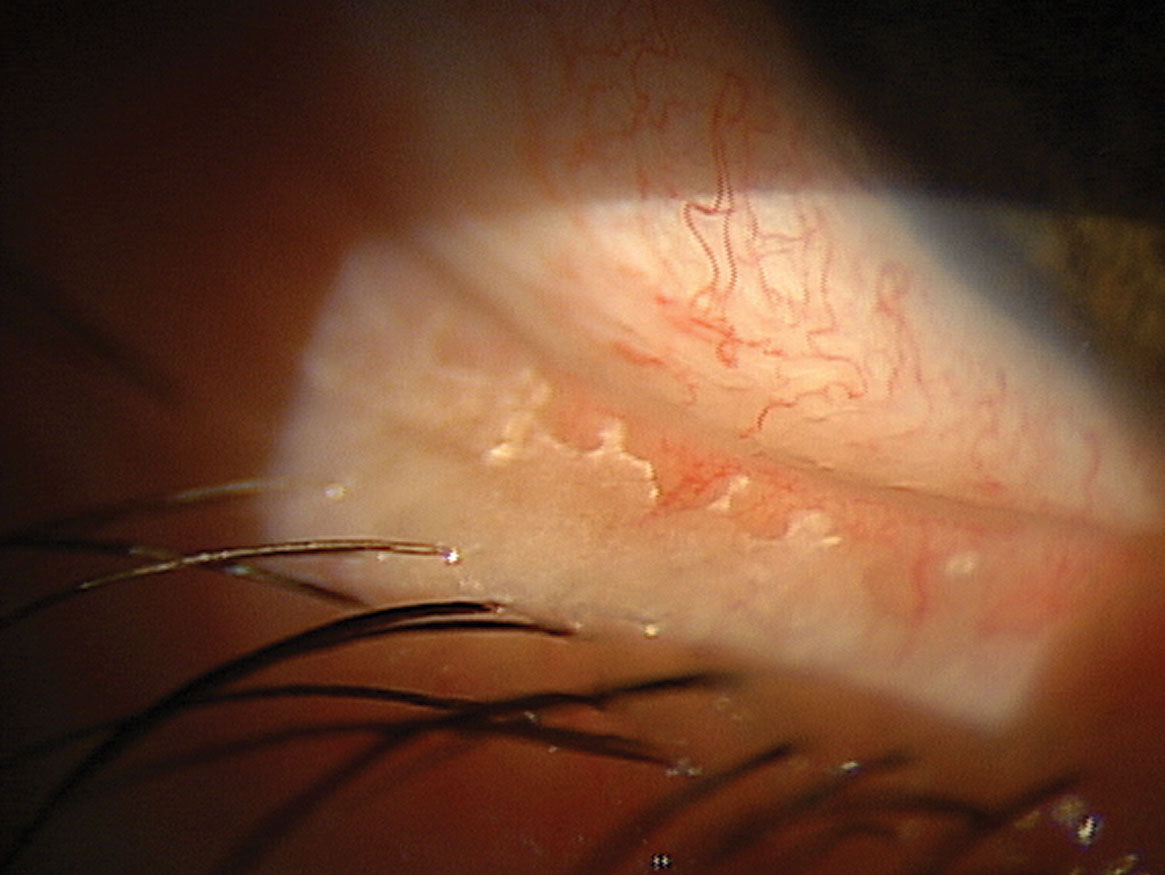 |
| Removing biofilm from the lid margin via Blephex reduces risk of blepharitis and dry eye as well. |
New to Market
Recently launched by Tear Film Innovations, iLux is a small, cost-effective in-office treatment for MGD that has a hand piece with a detachable, disposable, sterile tip and a magnifying lens. It is designed to provide better visualization of the blocked meibomian gland orifices and expressed meibum before and during the treatment. Once the LED-based heat source warms the inner and outer lids to a therapeutic temperature range, the clinician applies compression to express the melted meibum.
Based on the patient’s needs, the clinician can move the tip to different locations on the upper and lower lids and adjust the degree and duration of compression needed at each location. Most patients can be treated in under eight minutes.
In a randomized, open-label, multisite clinical trial comparing the iLux system to a predicate device, 142 patients were randomized between treatment options. Researchers looked at Meibomian Gland Score (MGS), TBUT and the Ocular Surface Disease Index (OSDI) questionnaire.
MGS improved from 5.6 prior to treatment with the iLux to 23.6 at week four, and tear-break-up time improved by more than 75% by week four; however, both improved as soon as two weeks. The OSDI scores also improved from more than 50 prior to treatment to about 20 by two weeks after treatment and improved further at four weeks.
Overall, both treatments produced statistically and clinically significant improvements in the signs and symptoms of MGD, meeting the FDA criteria for approval.
In the Pipeline
The TearCare system (Sight Sciences)—an in-office treatment that just debuted at the Academy of Optometry meeting and is being rolled out now—includes a single-use treatment kit that consists of four adhesive applicators that deliver heat (at 41°C to 45°C) to the external lids. The applicators are connected by a cable to a small, reusable handheld unit. Patients are instructed to blink normally during the 12-minute procedure to express meibum, and the clinician uses expression forceps afterwards to further evacuate the glands.
A prospective, randomized, pilot study demonstrated that the treatment had an immediate improvement on objective measures (TBUT, MGS and corneal and conjunctival staining) that was sustained through six months, while no such improvement was seen in the control group using daily at-home warm compresses with the washcloth bundle method.9
The More, the Merrier
In-office treatment for meibomian gland dysfunction can be a great service for patients who are suffering from the symptoms of MGD and dry eye disease. The importance of good eyelid health and hygiene provides comfort, reduces risk of blepharitis and protects the ocular surface from potential compromise. Care of the lids and meibomian glands can also help set your patients up for success when preparing for cataract or refractive surgery or experiencing decreased contact lens wearing time.
These treatments can also be an important new revenue source for an optometric practice. This is a great time to evaluate available and upcoming treatments to determine how they might best fit into your practice.
Note: Dr. Karpecki consults for a number of manufacturers with products relevant to this topic.
1. Lemp MA, Crews LA, Bron AJ, et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012:31(5):472-8. 2. Lane SS, DuBiner HB, Epstein RJ, et al. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea. 2012;31(4):396-404. 3. Blackie CA, Coleman CA, Holland EJ. The sustained effect (12 months) of a single-dose vectored thermal pulsation procedure for meibomian gland dysfunction and evaporative dry eye. Clin Ophthalmol. 2016;10:1385-96. 4. Greiner JV. Long-term (3-year) effects of a single thermal pulsation system treatment on meibomian gland function and dry eye symptoms. Eye Contact Lens. 2016;42(2):99-107. 5. Kading D. Presented at Vision Expo West (VEW), 2015; Las Vegas, NV. 6. Korb DR, Blackie CA. Debridement-scaling: A new procedure that increases meibomian gland function and reduces dry eye symptoms. Cornea. 2013;32(12):1554-7. 7. Rynerson JM, Perry HD. DEBS—a unification theory for dry eye and blepharitis. Clin Ophthalmol. 2016;10:2455-67. 8. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction; A 3-year retrospective study. Photomedicine and Laser Surgery. 2015;33(1):41-6. 9. Badawi D. A novel system, TearCare, for the treatment of the signs and symptoms of dry eye disease. Clin Ophthalmol. 2018;12:683-94. |

