|
|
 
|
Today, optometrists can access an impressive drug armamen-tarium to treat our patients. The anti-infectives, steroids, antihistamines and glaucoma medications currently available are second to none and represent a huge step forward from the options of only a few years ago. With the potency and efficacy of new therapies, often there comes a high price. Clinically, these new medications are outstanding, but when patients cannot afford them, how should an optometrist respond? Are clinicians justified in reaching back to an older, tried-and-true standby?
This month’s column is a “Throwback Thursday” edition (with author photos to match), wherein we’ll explore older medicines that still have a place today.
Infectious Bacterial Keratitis
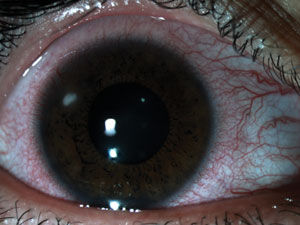
The first case we’ll look at involves a 45-year-old woman recently released from eight months of incarceration. A high myope, she never disclosed to prison officials that she wore soft contact lenses, and used a single pair of lenses incessantly for the duration. She presented with a painful, red, right eye. Her findings included profound conjunctival injection, a significant secondary anterior chamber reaction, dense paracentral corneal infiltration—which fortunately did not immediately threaten her visual axis—and epithelial excavation. In short, she had an infectious keratitis, presumably of bacterial nature.
|
|
|
Patient 1 presented with infectious keratitis, which responded to treatment with ofloxacin. Photo courtesy of Dr. Lori Vollmer
|
|
After explaining the diagnosis and risk of permanent vision loss, we discussed therapeutic options and the need for potent antibiotics. We felt that a fourth generation fluoroquinolone such as moxifloxacin, gatifloxacin or besifloxacin would be best. However, after discussing the cost of these branded medications, the patient emphatically stated that she would not be able to afford them and could not possibly use them. After a discussion about the need for aggressive treatment, a compromise was reached. We prescribed generic Ocuflox (ofloxacin 0.3%) which cost her about $9.00. Though Ocuflox is an older generation fluoroquinolone, it eradicated the infection successfully.
Ocuflox and Ciloxan
Ocuflox and Ciloxan (ciprofloxacin 0.3%) are second-generation fluoroquinolone antibiotics FDA approved for the topical treatment of bacterial conjunctivitis and bacterial keratitis caused by susceptible organisms. These medications have in vitro and in vivo activity against a broad range of gram-positive and gram-negative aerobic and anaerobic bacteria. Ofloxacin and ciprofloxacin are bactericidal at concentrations equal to or slightly greater than inhibitory concentrations. Ofloxacin and ciprofloxacin exert bactericidal effects on susceptible bacterial cells by inhibiting DNA gyrase (which is a type II topoisomerase) or topoisomerase IV, which is an enzyme necessary to separate replicated DNA, thereby inhibiting bacterial cell division, or both.
Topical Fluoroquinolones
The development in the 1990s of topical fluoroquinolones offered a highly effective alternative to fortified antibiotics for patients with bacterial keratitis. For the first time, commercially available antibiotics were scientifically compared with the standard treatment of fortified antibiotics. Historically, bacterial keratitis was treated with compounded, fortified solutions of aminoglycosides and cefazolins. Often, this involved diluting antibiotics originally designed for intravenous use. The results of the Bacterial Keratitis Study Group, as well as more recent studies, showed that ofloxacin and ciprofloxacin were equivalent to fortified cefazolin and tobramycin solutions in the management of patients with bacterial keratitis.1-5
The reduced frequency of ocular toxic effects and the relative ease of use of these fluoroquinolones was seen as additionally beneficial in these studies.
Efficacy
However, bacteria have grown increasingly resistant to second generation fluoroquinolones, and some researchers suggest that later generation fluoroquinolones, such as gatifloxacin 0.3%, provide superior coverage.6
Inspection of at least one medication pricing website,
www.goodrx.com, indicates that the cost of gatifloxacin 2.5ml is $131.28 for the branded form and $50.72 for the generic version. In comparison, 5ml of generic ofloxacin is $9.37 and generic ciprofloxacin is $11.74. Unquestionably, the fourth generation fluoroquinolones are outstanding in terms of antibiotic efficacy and superior choices for sight-threatening infections. But the most effective medication will not work if the patient can’t afford it. Don’t discount older generation fluoroquinolones. They remain effective and accessible to most patients.
Non-infecious Keratopathy
In another case, a 30-year-old female contact lens wearer presented with a red, moderately irritated right eye. She had diffuse injection of her bulbar conjunctiva and a non-staining peripheral corneal infiltrate. Additionally, she had a mild diffuse epitheliopathy. We diagnosed a contact lens-related hypoxia and non-infectious keratopathy. We told her to temporarily discontinue contact lens wear. We wanted to reduce inflammation while providing some degree of antibiotic coverage and recommended a combination antibiotic-steroid medication.
When she reported that she had no insurance, we again consulted www.goodrx.com to get an idea of her anticipated costs. We looked at two branded steroid-antibiotic combination agents and found that a 5ml bottle would cost her from $158.88 to $197.97. Her facial expression gave us her answer. We prescribed an alternative, generic Maxitrol solution, which she purchased for $4.00. Within a week, her condition resolved.
Maxitrol
Maxitrol is an antibiotic-steroid combination of neomycin sulfate 3.5mg, polymyxin B sulfate 10,000 units, and dexamethasone 0.1%. As with most antibiotic-steroid combinations, it is appropriate for steroid-responsive inflammatory ocular conditions for which a corticosteroid is indicated and where bacterial ocular infection or a risk of infection exists. Polymyxin B is an antibiotic used for resistant gram-negative infections, altering bacterial outer membrane permeability by binding to a negatively charged site in the lipopolysaccharide layer, which results in a destabilized bacterial outer membrane.
Neomycin is an aminoglycoside antibiotic that, like others in the category, has excellent activity against gram-negative bacteria, and has partial activity against gram-positive bacteria. It is relatively toxic. Much has been said about the potential allergic responses that patients have to neomycin, making it a lesser choice for clinicians. However, the majority of allergic reactions that we have seen have involved over-the-counter dermatologic preparations where patients used it off-label for the eyes. We cannot recall any instance where Maxitrol caused a toxic ocular reaction, quite possibly due to the steroid combating any allergic responses. Lately, we have seen more cataract surgeons providing Maxitrol in postoperative kits, likely due its efficacy and price. While branded antibiotic-steroid combinations are excellent choices, we never hesitate to prescribe Maxitrol.
Ocular Hypertension
The final patient is a 58-year-old male with ocular hypertension, also with no prescription drug coverage. His untreated IOP was 25mm Hg OD and 26mm Hg OS and his central cornea was thin at 456µm OD and 464µm OS. He mentioned his mother lost vision due to glaucoma. After a detailed discussion about the risks and benefits of prophylactic IOP reduction, we prescribed generic latanoprost, which gave him an unacceptable degree of hyperemia.
We discontinued the latanoprost and instead prescribed generic timolol 0.5%, which was tolerable and affordable at $4.00 a bottle. Using timolol, this patient achieved adequate IOP reduction.
Timolol
Since the advent of the prostaglandin medications, clinicians’ reliance on topical beta blocker therapy has significantly reduced. However, prior to the development of prostaglandins, doctors used beta blockers extensively with few problems. Like prostaglandin analogs, the earlier introduction of branded Timoptic (timolol maleate 0.5%) revolutionized glaucoma management.
While specific contraindications exist, it appears that many of the propagated fears about topical beta blockers stem from anecdotal case reports rather than evidence-based sources. These drugs are actually quite safe for the vast majority of patients, and virtually no confirmation shows they directly induce clinical depression, sexual dysfunction, claudication, prolonged hypoglycemia or hypoglycemic unawareness.7
However, practitioners must remain aware of potential complications and be alert for any unusual systemic complaints in patients using beta blocker therapy. Always obtain a thorough health history, check in-office pulse rate, and refer patients for medical evaluation when indicated prior to initiating topical beta blockers. With these minimal precautions appropriately taken, timolol is an excellent first-line medication, which gives impressive IOP reduction at a low cost.
The field has developed a number of ophthalmic medications in the last several years with unprecedented efficacy. However, it is important to remember medications we used successfully in the past. Just because something is old doesn’t mean it isn’t good.
The authors would like to thank Dr. Amanda Brown for suggesting this column.
1. O’Brien TP, Maguire MG, Fink NE, et al. Efficacy of ofloxacin vs cefazolin and tobramycin in the therapy for bacterial keratitis. Report from the Bacterial Keratitis Study Research Group. Arch Ophthalmol. 1995;113(10):1257-65.2. The Ofloxacin Study Group. Ofloxacin monotherapy for the primary treatment of microbial keratitis: a double-masked, randomized, controlled trial with conventional dual therapy. Ophthalmology. 1997;104(11):1902-9.
3. Hyndiuk RA, Eiferman RA, Caldwell DR, et al. Comparison of ciprofloxacin ophthalmic solution 0.3% to fortified tobramycin-cefazolin in treating bacterial corneal ulcers. Ciprofloxacin Bacterial Keratitis Study Group. Ophthalmology. 1996;103(11):1854-62.
4. Khokhar S, Sindhu N, Mirdha BR. Comparison of topical 0.3% ofloxacin to fortified tobramycin-cefazolin in the therapy of bacterial keratitis. Infection. 2000;(3):149-52.
5. McDonald EM, Ram FS, Patel DV, McGhee CN. Topical antibiotics for the management of bacterial keratitis: an evidence-based review of high quality randomised controlled trials. Br J Ophthalmol. 2014;98(11):1470-7.
6. Parmar P, Salman A, Kalavathy CM, et al. Comparison of topical gatifloxacin 0.3% and ciprofloxacin 0.3% for the treatment of bacterial keratitis. Am J Ophthalmol. 2006;141(2):282-286.
7. Lama PJ. Systemic adverse effects of beta-adrenergic blockers: an evidence-based assessment. Am J Ophthalmol. 2002;134(5):749-60.

