 |
Q: Descemet’s membrane endothelial keratoplasty (DMEK) seems to be the lamellar procedure of choice these days for corneal endothelial disease. Can you describe the use of artificial materials that have recently been reported and who would be the best candidate for each device?
A: “Corneal endothelial disease, such as Fuchs’ endothelial dystrophy, posterior polymorphous dystrophy and iridocorneal endothelial syndrome, can lead to significantly impaired vision and quality of life,” says Christopher Lopez, OD, who practices in Wisconsin. “Fortunately, continued technological advancement has led to an improvement in treatment and management options.”
Current Options
 |
|
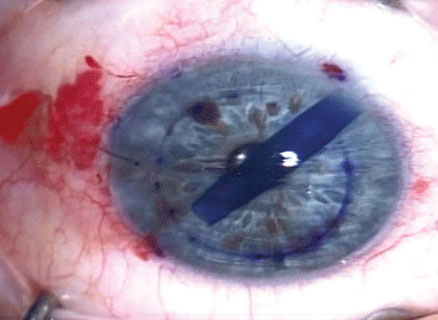
During DMEK, donor Descemet’s membrane tissue is stained with trypan blue for better visualization of the eye. Image courtesy of Aaron Bronner, OD. Click image to enlarge. |
Penetrating keratoplasty (PKP) used to be the primary surgical option for patients suffering from endothelial dysfunction. A PKP involves a full-thickness corneal tissue replacement with an allograft corneal button to replace damaged endothelial cells. Although its use has dwindled in favor of other techniques, PKP is still a contender under certain circumstances, especially when a patient has significant endothelial compromise.
Descemet’s stripping endothelial keratoplasty (DSEK) is often favored over PKP in mild-to-moderate cases of endothelial dysfunction. A DSEK involves replacing the posterior cornea with donor tissue consisting of endothelial cells, Descemet’s membrane and a portion of the posterior stroma. DSEK eyes tend to have favorable outcomes, with lower graft rejection rates, quicker visual recoveries and more predictable refractive endpoints compared with PKP eyes.
DMEK is similar to DSEK, with the distinction that DMEK donor grafts consist of healthy endothelial cells and Descemet’s membrane without posterior stromal tissue. DMEK outcomes favor better visual acuity and even lower rejection rates than DSEK.
Descemetorhexis without endothelial keratoplasty (DWEK) is a newer technique in the rehabilitation of corneas with endothelial compromise. DWEK consists of removing Descemet’s membrane without replacement with a donor graft. After the central area of Descemet’s membrane is surgically stripped away, healthy peripheral endothelial cells should migrate centrally to replace the removed cells. The goal is to improve corneal clarity and, therefore, enhance visual acuity.
Future Advancements
New research is exploring additional avenues for patients with corneal endothelial dysfunction. For example, stem cells have been engineered to replace the corneal endothelium.1 Rho-kinase (ROCK) inhibitors have demonstrated enhancement of endothelial cells.2 Additionally, endothelial cells can be multiplied and used in conjunction with ROCK inhibitors to increase endothelial cell count.3 Due to a worldwide shortage of tissue, several research centers are investigating artificial corneas. These areas of research show promising results but warrant further studies before they potentially evolve into mainstay treatments in the management of endothelial disease.
Takeaways
As with all of these procedures, proper patient selection is crucial in successfully improving corneal endothelial compromise. Additionally, each surgical technique has its own pros and cons. Gone are the days in which every patient undergoing corneal endothelial surgery is treated with a PKP. Scientific advancements have led to better surgical techniques with improved visual outcomes and enhanced safety profiles.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Yamashita K, Inagaki E, Hatou S, et al. Corneal endothelial regeneration using mesenchymal stem cells derived from human umbilical cord. Stem Cells Dev. 2018;27(16):1097-108. 2. Okumura N, Kinoshita S, Koizumi N. Application of rho kinase inhibitors for the treatment of corneal endothelial diseases. J Ophthalmol. 2017;2017:2646904. 3. Stephenson M. The newest treatment options for Fuchs’. Rev Ophthalmol. 2018;25(11):38-40. |

