 |
Numerous systemic conditions can manifest in the eye. In addition to clinical presentation, laboratory testing is often used in an ophthalmic setting to determine any underlying disease process and employ appropriate treatment strategies. Often, timely and accurate management of said conditions are necessary to prevent permanent vision loss. As such, initiating and interpreting lab tests is essential to determine a diagnosis and subsequent plan.
Infectious disease processes are often difficult to distinguish because of overlapping clinical features. A prime example is tuberculosis (TB), which may cause a range of ocular findings and is necessary to distinguish from other types of infection, as it can exhibit similar signs.1 There are a number of supporting ancillary tests to consider when making this diagnosis. Recognizing the mechanisms, indications and drawbacks of each test allows them to be used most effectively.
 |
| The TB skin test works by measuring a hypersensitivity reaction to the tuberculin protein, injected in the forearm. Click image to enlarge. |
On the Rise
TB is one of the leading causes of death worldwide and affects nearly a third of the world’s population.2 While the overall incidence of TB has been declining, there has been a re-emergence of infection, particularly in the developing world, caused by increased multi-drug resistance, poor socioeconomic conditions and global migration.2,3 Consequently, it remains a major public health concern and serious consideration to eyecare practitioners.3
TB arises from the infection of Mycobacterium tuberculosis, an obligate aerobic bacterium evident in tissues with high oxygenation. As such, the most common location of TB infection is in the lungs. The choroid, which is one of the most oxygenated tissues in the body, predisposes the eye to exhibit TB manifestations as well.2 Ocular TB can be caused by either primary or secondary infection of Mycobacterium. Most commonly, ocular TB occurs as a secondary manifestation of the bacteria through seeding and hematogenous spread from a distant site.
What makes the eye susceptible is its highly vascular nature, particularly the uveal tract, consisting of the iris, ciliary body and choroid.2,3 Another secondary form of ocular infection is through contamination of the patient’s own sputum. Primary exogenous spread of ocular TB is rare and manifests more in external ocular tissues and the anterior segment. There is another form of ocular TB that is secondary to hypersensitivity reaction, such as phlyctenular and Eales’ diseases.3
 |
| Click table to enlarge. |
TB or Not TB?
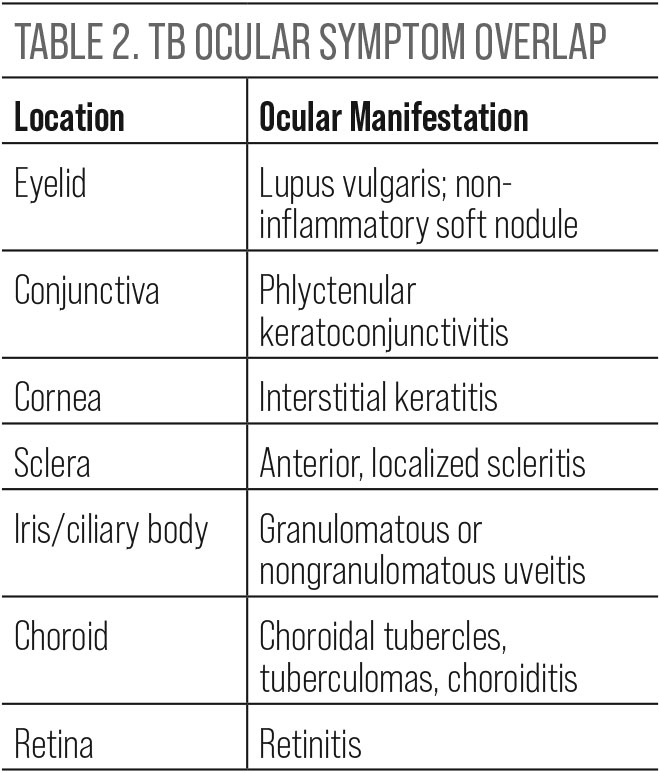
Ocular manifestations of TB affect all areas of the eye and often overlap with clinical findings common to other infectious or inflammatory conditions.
Adnexa. Externally, lid lesions can develop and appear as a soft, non-inflammatory mass in children. Another TB-specific lid lesion is lupus vulgaris, which is a reddish-brown mass that blanches upon pressure.
Conjunctiva. Involvement here can present with non-specific redness, mucopurulent discharge and lymphadenitis. Phlyctenular keratoconjunctivitis is a more specific finding, appearing as a small pink nodule at the limbus, which may later migrate onto the corneal surface, thereby leading to an epithelial defect. This form of keratoconjunctivitis indicates hypersensitivity to TB, which must be ruled out if present.
Cornea. In addition to phlyctenular keratoconjunctivitis, interstitial keratitis can also be a sign of ocular TB. It will appear as stromal corneal vascularization. Unlike phlyctenulosis, though, interstitial keratitis can occur from other types of infection. With TB, it is characteristically unilateral and confined to a sector of the corneal periphery.
Sclera. Refractory anterior scleritis cases should be evaluated for ocular TB infection. Typically, this form of scleritis manifests as a localized, dark red area with granulomatous inflammation and necrosis. Very rarely, the posterior sclera may also be inflamed.
Uvea. A well-known cause of granulomatous uveitis is TB. This includes clinical findings such as mutton fat keratic precipitates and Koeppe or Busacca nodules on the iris. Non-granulomatous presentations are also possible.
Choroid. The choroid, due to its high vascularization, is a common and unique site of ocular TB. The spectrum of choroidal involvement includes choroidal tubercles, tuberculomas and choroiditis. Choroidal tubercles are the most common ocular manifestation of ocular TB. These lesions are white, gray or yellow with indistinct borders measuring from 0.5mm to 3.0mm in diameter. They are located in the posterior pole and may lead to exudate formation, hemorrhages or edema. Due to the specificity of these lesions in association with TB, they should be very carefully looked for in patients who have a fever of unknown origin or other suspicious symptoms. Tuberculomas are similar in appearance but larger, measuring up to 7mm in diameter. They are usually a sole nodule with more distinct borders. Choroiditis in TB can be multifocal or serpiginous-like.
Retinitis. Tuberculous retinitis can appear as localized tubercles or diffuse inflammation. Associated features are vitreous opacification and retinal vasculitis. Neovascularization and peripheral capillary occlusion may also result. Retinitis of this nature can either be to the infection in the underlying choroid or hematogenous spread. Eales’ disease has also been associated with TB.1,2
 |
| Click table to enlarge. |
Diagnosing
When ocular TB is suspected, there is no definitive gold standard of testing. Diagnostic challenges arise from the impractical and invasive nature of culture biopsies from ocular fluids.2 Besides the unique ocular features, supplemental testing can help confirm the diagnosis, which is imperative to initiate proper treatment and reverse findings. Patients with accompanying pulmonary symptoms may benefit from chest radiography to confirm diagnosis. In the absence of pulmonary manifestations or even for confirmation, laboratory tests are often acquired.3
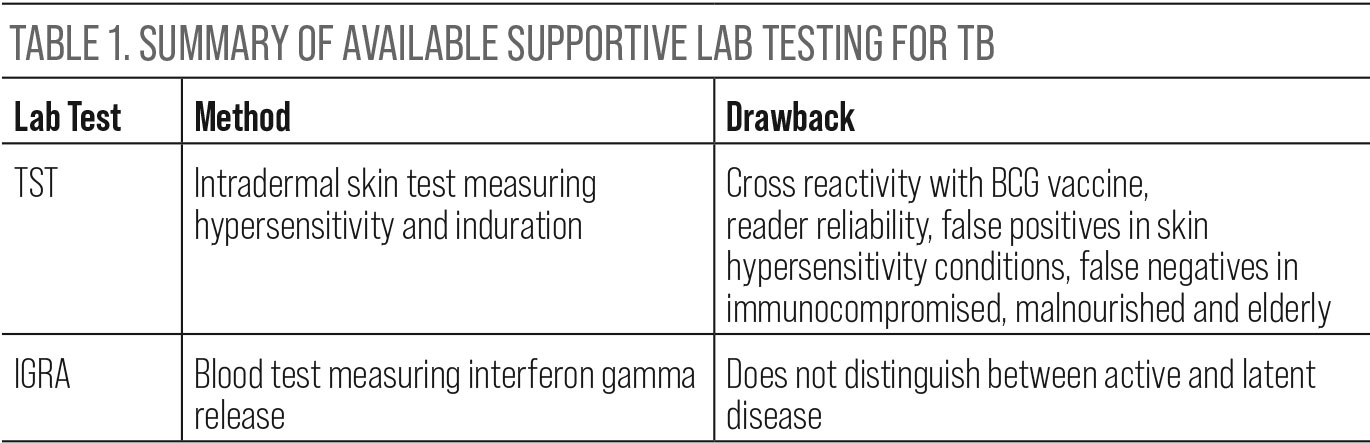
TB skin testing (TST) has long been used as a screening test for TB. The way this test works is through measurement of the hypersensitivity reaction to the tuberculin protein. This protein is extracted from M. tuberculosis and is used as a purified protein derivative. It is then injected intradermally on the surface of the forearm, where the type IV hypersensitivity reaction is then measured 48 to 72 hours later. This reaction appears as erythema and induration. The induration, or palpable raised swelling, is measured. A positive test is a measurement of 10mm or larger.2,3
The drawback to this test is that it is time sensitive and requires accurate reading. Furthermore, false positive tests can occur in patients who have previously been vaccinated for Bacille Calmette–Guerin (BCG), which is a nontuberculous mycobacterium. Additional false positives can arise in patients who have excessive skin hypersensitivities, such as in Behçet’s disease. False negatives are just as possible and occur more so in elderly, malnourished or immunocompromised patients.4
More recently, blood testing using interferon-gamma release assay (IGRA) such as QuantiFeron TB gold, has been used in the diagnosis of TB. Similar to the TST, this test also works through cell-mediated immunity secondary to TB exposure. As the name suggests, this blood test measures interferon gamma release by antigen specific T-cells in response to TB antigens. It is preferred over the TST because it does not have the same drawbacks of cross reactivity with the BCG vaccine and does not require the same timeliness and reliability of the reader. Both forms of testing, however, do not have the ability to distinguish between active and latent forms of TB.4,5
While TST has been the mainstay of TB testing for decades, the clinical utility of IGRA has substantially impacted the diagnosis of disease in recent years. Since ocular manifestations of TB are common and variable, the mechanism of infection, clinical manifestations and supporting laboratory tests must be widely understood in order to form an early diagnosis. Timely intervention with systemic TB treatment can reverse many of these ocular manifestations and preserve vision.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Albert DM, Raven ML. Ocular tuberculosis. Microbiol Spectr. 2016;4(6):10.1128/microbiolspec.TNMI7-0001-2016. 2. Shakarchi FI. Ocular tuberculosis: current perspectives. Clin Ophthalmol. 2015;9:2223-7. 3. Pahal P, Sharma S. PPD skin test. 2022 Jan 24. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 4. Shafeque A, Bigio J, Hogan CA, Pai M, Banaei N. Fourth-generation QuantiFERON-TB Gold Plus: What is the evidence? J Clin Microbiol. 2020;58(9):e01950-19. 5. Anwar A, Hamdan AJ, Salim B, et al. Diagnostic utility of QuantiFERON-TB Gold (QFT-G) in active pulmonary tuberculosis. J Glob Infect Dis. 2015;7(3):108-12. |

