 |
Darwin noted that those who are best able to adapt are the ones who survive. So it’s no surprise that much of a clinician’s success can be attributed to their ability to adapt to change; in optometry, this requires time, research, observation and evidence. When all of this leads to improved patient care and more effective management, the new way of thinking takes hold.
Two recent major changes from traditional thinking stand out. First is the realization that dry eye disease (DED) is often asymptomatic, and, second, osmolarity testing is not just a number used for patient compliance purposes; it can actually change the diagnosis and treatment plan.
For decades we’ve been taught that dry eye is a symptomatic disease and treatment will make your patients happy. Yet, research suggests that relying on symptoms to diagnose DED would produce an incorrect diagnosis over 40% of the time.1-3 Imagine if you had to remake spectacles over 40% of the time—it’d be hard to build a practice on a process that error prone; it’s the same with building an OSD or DED practice.
Signs vs. Symptoms
So why is there such a disparity between signs and symptoms? Research shows that we may not be asking all the right questions; for example, we rarely ask about blurred vision, yet it is one of the most consistent symptoms of DED in all severity levels.4 Additionally, although tear fluid hyperosmolarity initially increases nerve activity of cold thermoreceptor endings in the cornea, leading to symptoms of dryness, chronic dry eye disease shows that symptoms dissipate as the disease progresses and corneal hypoesthesia develops.5,6 If inflammation-induced hypersensitivity to polymodal or cold receptors occurs, patients may develop a neuropathic dry eye, which is extremely difficult to manage.7 To make DED symptomatology even more complex, Sjögren’s syndrome patients with longstanding aqueous tear deficiency and keratoconjunctivitis sicca (KCS) have reduced corneal sensitivity, yet they still complain of more irritation than other longstanding DED patients.8
Because DED symptoms go through a cycle, a patient whose inflammation is not addressed (e.g., uses only OTC artificial tears) during the symptomatic phase of the disease may actually progress until the nerves are altered or downregulated, causing the patient to believe the disease has resolved. In actuality, it has likely progressed and the patient will only seek help when vision is significantly decreased due to advanced DED signs. These patients are not mentioning dryness, burning, grittiness or any typical dry eye symptoms, making it difficult to diagnose correctly.
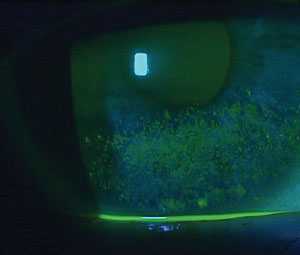 | |
| Corneal staining is a late-stage disease indicator. |
With chronic inflammation, alterations in corneal nerve morphology develop, including thicker appearing stromal nerves (but no increase in nerve density) and nerve growth of cone-like structures often associated with dendritic antigen-presenting cells, thus implicating longstanding inflammation as a cause.6-8 If it persists long enough, neuropathic pain, potentially involving the central and peripheral trigeminal sensory network, may develop.9
Additionally, symptoms that mimic dry eye disease can be caused by numerous conditions, including asthenopia from vertical imbalance, convergence insufficiency or fixation disparity, Salzmann’s nodular degeneration, recurrent corneal erosion, giant papillary conjunctivitis, allergic conjunctivitis, bacterial or viral conjunctivitis, blepharitis, pinguecula, conjunctivochalasis, etc.10-24 Many of these conditions involve symptoms of gritty, dry, burning eyes that give the impression of DED, based on a symptomatic approach, yet the causes and management are entirely different.
Osmolarity Testing
One test that may help make the DED diagnosis without relying on symptoms alone is osmolarity testing. Although there are over 2,000 studies on osmolarity and the ocular surface, with the majority of them (>90%) supporting the technology in DED management, many doctors remain unsure of its applications and how, or even if, it benefits clinical care.25
Although most clinicians will state that it is mainly used to monitor disease progression and provide a number to assist patient compliance, I disagree. The primary purpose of tear osmolarity testing is to know if a patient has dry eye disease. Hyperosmolar status, whether through decreased tear production or an increased evaporative state, indicates reduced aqueous levels.26 The test indicates whether or not the patient has a higher salt content than normal: as the volume of aqueous declines, the salt concentration in tears increases. When using osmolarity testing in a new, untreated patient, if you get a reading under 290mOsmol/L and each eye is within 8mOsmol/L of the other (e.g., osmolarity of 281 and 285), the patient likely doesn’t have dry eye disease.27 Don’t start them on steroids, Restasis (cyclosporine ophthalmic emulsion, Allergan) or even artificial tears. Instead, look for other causes such as the various forms of conjunctivitis, conjunctivochalasis or eye alignment issues like vertical disparity or fixation/proprioceptive disparity between the eyes.
A recent patient with symptoms of dry eyes, grittiness and burning, which were worse while working on a computer or late in the day, tested positive for inferior corneal staining, a rapid tear break-up time and a small tear meniscus. She was put on topical steroids, Restasis and artificial tears, but reported no improvement after six months and discontinued all her drops. Four months later, she was observed in our clinic and osmolarity was measured at 287 and 289—no dry eye. Demodex blepharitis and vertical phorias were diagnosed. Both conditions were treated, and symptoms fully resolved. Without osmolarity testing, patients such as this one are often prescribed drops for months or years to treat DED. It is only after therapies fail do we decide they don’t have DED. I’d rather perform osmolarity testing and know the answer in seconds on the first evaluation.
Treating DED
Knowing patients’ osmolar status can also help with treatment options. Anecdotally, through a registry of hundreds of patients, we have determined that a patient with elevated osmolarity (i.e., >320) and any level of MGD is going to respond better to a tear that lowers osmolarity more than others, such as Blink (Abbott Medical Optics) or TheraTears (Akorn), and will typically choose it over a lipid-based tear.28-30 By contrast, a patient with <310 osmolarity and mild to moderate MGD will often choose a lipid-based tear—such as Retaine MGD (Ocusoft), Refresh Optive Advanced (Allergan), Systane Balance (Alcon), Soothe XP (Bausch + Lomb)—the majority of the time. Gauge the level of MGD to determine which direction to go with patients between 310 and 320.31 Even my choice of artificial tears depends on osmolarity, MG expression and analysis.
Inflammation must be treated at all levels of DED, given the effects on symptoms and progression of the disease, but higher osmolarity measurements require more aggressive therapy. If you use topical corticosteroids and Restasis, you must alter treatment if osmolarity is not improved at two months. If osmolarity does improve but symptoms do not, you can feel confident that it’s the right treatment and the patient will eventually show improvement in symptoms.32 Proper patient education about the benefits of the right treatment will keep patients engaged in their care. It also helps with compliance when patients see a quantifiable improvement. Without osmolarity, as DED management stands now, a patient would either stay on the drop unnecessarily—even if it is doing nothing—or stop prematurely because the symptoms haven’t improved, even though it’s the correct treatment and just needs more time. Neither is ideal.
I have had many cases where osmolarity completely changed my dry eye management plan. Recently, I saw a patient with osmolarity of 287 and 284, with all the classic symptoms of dry eye disease. The osmolarity number prompted me to look elsewhere for the cause of discomfort. I everted the eyelid and there was a large concretion, which I only noticed on double eversion because it was at the tarsal plate margin edge. After its removal, the patient’s symptoms resolved completely. He’d been treated for DED with artificial tears, topical steroids, Restasis and doxycycline for over eight months. The osmolarity readings increased my suspicion of a diagnosis other than DED.
Keep in mind that a normal osmolarity reading could also mean a DED patient that is well treated and the disease is controlled or homeostasis maintained.26 Also, osmolarity testing should not be used in isolation; it must be combined with other findings. No one test works 100% of the time. Osmolarity may be the most accurate predictor of DED or severity of disease, but when you start combining tests (e.g., osmolarity + MG expression + corneal staining + symptoms, etc.), you begin to see a significant improvement in sensitivity and specificity of the disease diagnosis and management plan.27,33
Dr. Karpecki has a financial relationship with AcuFocus, AMO, Alcon Labs, Allergan, Akorn, Bausch + Lomb/Valeant, BioTissue, Bruder Healthcare, Cambium Pharmaceuticals, Eleven Biotherapeutics, Eyemaginations, Essilor, Fera Pharmaceuticals, Focus Laboratories, iCare USA, Ocusoft, Freedom Meditech, Konan Medical, Beaver-Visitech, Eye Solutions, Reichert, Shire Pharmaceuticals, RySurg, Science Based Health, SightRisk, TearLab, TearScience, TLC Vision, Topcon and Vmax.
1. Bron AJ, Tomlinson A, Foulks GN, et al. Rethinking dry eye disease: a perspective on clinical implications. Ocul Surf. 2014Apr;12(2 Suppl):S1-31.
2. Sullivan BD, Crews LA, Messmer EM, et al. Correlations between commonly used objective signs and symptoms for the diagnosis of dry eye disease: clinical implications. Acta Ophthalmol. 2014 Mar;92(2):161-6.
3. Fuerst N, Langelier N, Massaro-Giordano M. Tear osmolarity and dry eye symptoms in diabetics. Clin Ophthalmol. 2014 Mar;8:507-15.
4. Iyer JV, Lee SY, Tong L. The dry eye disease activity log study. Scientific World Journal. 2012;2012:589875.
5. Parra A, Gonzalez-Gonzalez O, Gallar J, Belmonte C. Tear fluid hyperosmolality increases nerve impulse activity of cold thermoreceptor endings of the cornea. Pain. 2014 Aug;155(8):1481-91.
6. Bourcier T, Acosta MC, Borderie V, et al. Decreased corneal sensitivity in patients with dry eye. Invest Ophthalmol Vis Sci. 2005 Jul;46(7):2341-5.
7. Belmonte C, Acosta MC, Merayo-Lloves J, et al. What causes eye pain? Curr Ophthalmol Rep. 2015;3(2):111-21.
8. Tuisku IS, Konttinen YT, Konttinen LM, et al. Alterations in corneal sensitivity and nerve morphology in patients with primary Sjögren’s syndrome. Exp Eye Res. 2008 Jun;86(6):879-85.
9. Rosenthal P, Borsook D. Ocular neuropathic pain. Br J Ophthalmol. 2015 May 5.
10. Thorud HM, Helland M, Aarås A, et al. Eye-related pain induced by visually demanding computer work. Optom Vis Sci. 2012 Apr;89(4):E452-64.
11. Iwasaki T, Tawara A. Eyestrain induced by stereogram on 3-D display—differences between types of correction. Nihon Ganka Gakkai Zasshi. 2002 Jul;106(7):404-10.
12. Hurmeric V, Yoo SH, Karp CL. In vivo morphologic characteristics of Salzmann nodular degeneration with ultra-high-resolution optical coherence tomography. Am J Ophthalmol. 2011 Feb;151(2):248-56.
13. Azari AA, Rapuano CJ. Autologous serum eye drops for the treatment of ocular surface disease. Eye Contact Lens. 2015 May;41(3):133-40.
14. Asbell PA, Torres MA. Drugs. Therapeutic dilemmas in external ocular diseases. 1991 Oct;42(4):606-15.
15. Chiambaretta F, Gerbaud L, Fauquert JL. Management of allergic conjunctivitis. An observational study among ophthalmologists. J Fr Ophtalmol. 2014 Jan;37(1):9-17.
16. Siedman MD, Gurgel Rk, Ln SY, et al. Clinical practice guideline: allergic rhinitis. Otolarygol Head Neck Surg. 2015 Feb;152:S1-43.
17. Lar Ros M, Lionetti E, Beibaldi M, et al. Allergic conjunctivitis: a comprehensive review of the literature. Italian journal of Pediatrics. 2013;39:18.
18. Leonardi A, Pileigo F, Castegnaro A, et al. Allergic conjunctivitis: a cross-sectional study. Clin Exp Allergy. 2015 June;45(6):1118-25.
19. Narayana S, McGee S. Bedside diagnosis of the Red Eye: A systematic review. Am J Med. 2015 Jul;S2-9343(15):00577.
20. Weber CM, Eichenbaum JW. Acute red eye. Differentiating viral conjunctivitis from the other less common causes. Postgrad Med. 1997 May;101(5):185-6.
21. Pihos AM. Epidemic keratoconjunctivitis: A review of current concepts in management. J Optom. 2013;6:69-74.
22. Guillon M, Maissa C, Wong S. Symptomatic relief associated with eyelid hygiene in anterior blepharitis and MGD. Eye Contact Lens. 2012 Sep;38(5):306-12.
23. Balci O. Clinical characteristics of patients with conjunctivochalasis: Clin Ophthalmic. 2014 Aug 28;8:1655-60.
24. Di Pascuale MA, Espana EM, Kawakita T, Tseng SC. Clinical characteristics of conjunctivochalasis with or without aqueous tear deficiency. Br J Ophthalmol. 2004 Mar;88(3):388-92.
25. McMonnies CW. An examination of the relationship between ocular surface tear osmolarity compartments and epitheliopathy. Ocul Surf. 2015 Apr;13(2):110-7.
26. Baudouin C, Aragona P, Messmer EM, et al. Role of hyperosmolarity in the pathogenesis and management of dry eye disease: proceedings of the OCEAN group meeting. Ocul Surf. 2013 Oct;11(4):246-58.
27. Keech A, Senchyna M, Sullivan BD, et al. Impact of time between collection on human tear film fluid osmolarity. Invest Ophthalmol Vis Sci. 2010;51:E-abstract 4174. 28. Nelson JD, Farris RL. Sodium hyaluronate and polyvinyl alcohol artificial tear preparations. A comparison in patients with keratoconjunctivitis sicca. Arch Ophthalmol. 1988;106:484-7.
29. Gilbard JP, Rossi SR, Heyda KG. Ophthalmic solutions, the ocular surface, and a unique therapeutic artificial tear formulation. Am J Ophthalmol. 1989 Apr 15;107(4):348-55.
30. Gilbard JP. Dry eye: pharmacological approaches, effects, and progress. CLAO J. 1996 Apr;22(2):141-5.
31. Scaffidi RC, Korb DR. Comparison of the efficacy of two lipid emulsion eyedrops in increasing tear film lipid layer thickness. Eye Contact Lens. 2007 Jan;33(1):38-44.
32. Sullivan BD, Crews LA, Sönmez B, et al. Clinical utility of objective tests for dry eye disease: variability over time and implications for clinical trials and disease management. Cornea. 2012 Sep;31(9):1000-8.
33. Sullivan BD, Whitmer D, Nichols KK, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010 Dec;51(12):6125-30.

