 |
|
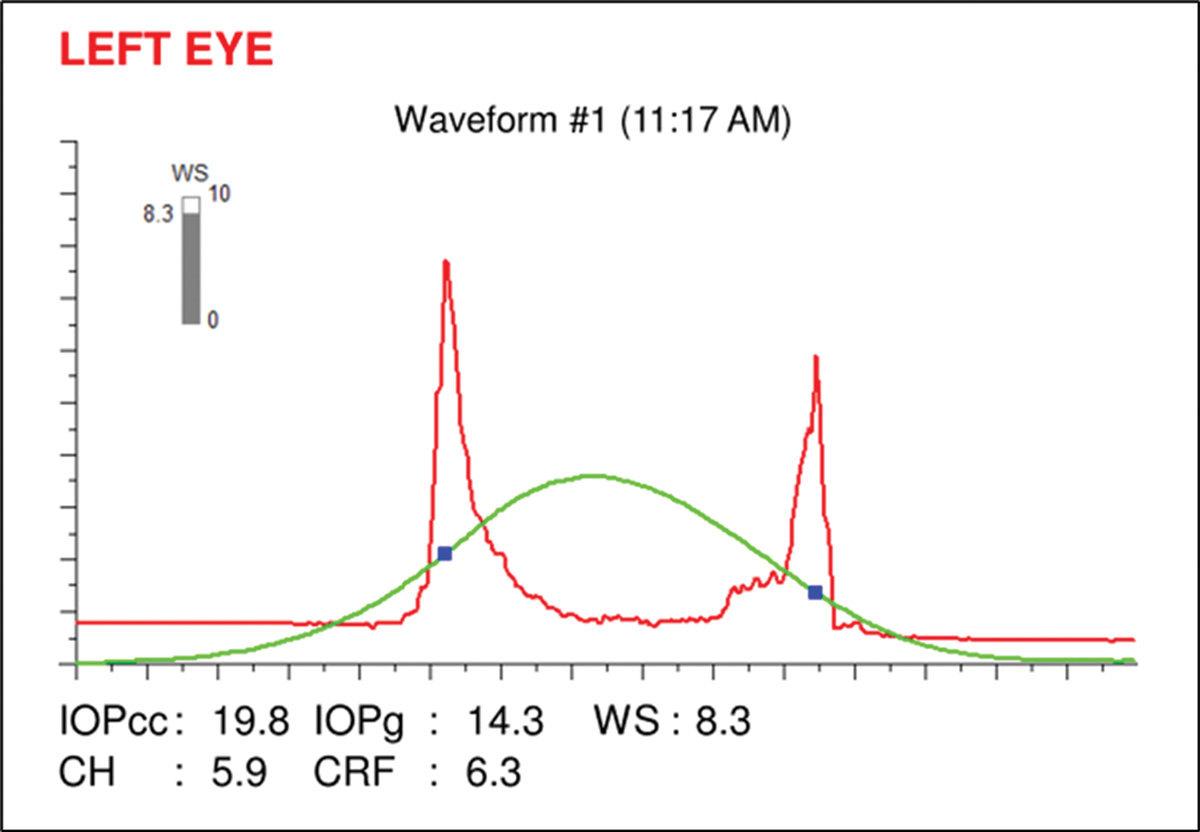
Although various forms of glaucoma can result in lower hysteresis values, interpretation of CH measurements in an individual patient is complicated by IOP effects, study finds. Photo: Sarah B. Klein, OD. Click image to enlarge. |
While intraocular pressure (IOP) is central to the diagnosis and treatment of glaucoma, its significance is likely overstated, due to the dearth of other easy-to-obtain biomarkers. For years, proponents have argued that corneal hysteresis (CH) adds much-needed nuance to the clinical apprehension of IOP and hence the patient’s glaucoma status. To help, the American Academy of Ophthalmology recently weighed in, issuing one of its Ophthalmic Technology Assessment papers on the topic.
An expert panel reviewed published literature on the utility of CH in diagnosing glaucoma and assessing the disease’s progression in existing patients with glaucoma. Data was gathered through searching peer-reviewed literature in the PubMed database. Included in the retrospective analysis were 19 articles, rated for level of evidence by the panel methodologist. Eight were rated level I and five were rated level II.
The researchers broke the articles down into two general categories: CH use in glaucoma screening and in disease development/progression. CH values between normal and glaucomatous eyes were further subdivided into different glaucoma types, including primary open-angle glaucoma (POAG), primary angle-closure glaucoma (PACG), pseudoexfoliative glaucoma, normal-tension glaucoma (NTG) and ocular hypertension.
After reviewing the articles included, the researchers came to find that corneal hysteresis was lower in patients with POAG, PACG, pseudoexfoliative glaucoma and pseudoexfoliation syndrome when compared to normal, control eyes. Even further, lower hysteresis values were associated with an increased risk of disease progression.
Determining the significance of a lower observed CH is complicated by patients with higher IOP or who are on topical hypotensive medication, because these confounding factors influence the parameters of CH measurements. Despite this, CH was additionally observed to be lower in treatment-naïve, NTG patients compared to controls with similar IOP.
Out of the five articles that looked at POAG, four indicated level I evidence and four found that POAG patients had lower CH compared to controls. Four articles compared CH with PACG patients, all providing level I evidence. Within this subgroup, limitations existed between with different IOP levels between groups and the effects that topical hypotensive medications may have on hysteresis.
Three articles were included looking at CH in psedoexfoliative glaucoma or pseudoexfoliation syndrome, all providing level II evidence. All three found lower CH with pseudoexfoliative glaucoma, while patients with pseudoexfoliative syndrome (without glaucoma evidence) displayed higher CH than pseudoexfoliative glaucoma patients but lower CH than normal controls.
Two articles were included in the NTG subgroup, both providing level I evidence. This subgroup also proved interesting because untreated NTG can be matched to healthy eyes for IOP, effectively getting rid of confounding factors of IOP and topical hypotensive medication. With that possibility, both of the articles found lower CH in NTG compared to controls.
Despite the consensus across all subgroups displaying lower CH, the authors caution that “interpretation of CH measurements in an individual patient is complicated by IOP effects as well as medical, laser and surgical therapy, and other influencing parameters such as age, CCT and axial length.”
The authors still posit that, “nevertheless, most evidence suggests that the CH measurement is a potential adjunct in identifying glaucoma patients and those who may be at increased risk for disease progression” and that the measurement of CH “complements current structural and functional assessments in determining disease risk in glaucoma suspects and patients.”
Sit AJ, Chen TC, Takusagawa HL, et al. Corneal hysteresis for the diagnosis of glaucoma and assessment of progression risk. Ophthalmol. 2022. [Epub ahead of print]. |

