 |
One of the most difficult things to teach optometry students is how to choose a final spectacle prescription. They learn quickly how to perform a manifest refraction, how to do a binocular balance and how to determine best acuity through the proposed lenses; this is all fairly easy to teach. What is harder to convey, though, is how to pick the best Rx for a patient—which lenses will that patient actually be able to use comfortably and efficiently to fulfill their visual goals? It’s not always the numbers that are shown through our testing.
A prime example of this that we have noticed over our 20+ years in optometric education is in helping students learn what to do with small amounts of cylinder. It is easy to define refractive conditions by a simple mathematical combination of the refractive power of the cornea, lens and length of the globe. As these values are relatively constant for a given individual, though, how do we account for the small fluctuations in refractive status that we see as we go through our standard testing? What does it mean when a patient shows something different following dilation or cycloplegia? There are underlying functional phenomena that can account for this, and it is important that we test for and pay attention to these when prescribing.
Discussion
I (Dr. Schnell) am fascinated by history, particularly by the history of our own profession, so I tend to read papers and books by some of the foundational minds in optometry. If we dig back into the work of several well-known optometrists—A. M. Skeffington and Elliott Forrest are two whose work continues to inspire me—we can find explanations of what is happening when we see transient astigmatism in our patients.
According to Dr. Forrest, functional astigmatism is indicated when patients move their eyes more in a given direction than they do their head.1 Thus, small amounts of with-the-rule astigmatism are seen in patients who tend to move their eyes side-to-side more, and low against-the-rule cylinders appear in patients whose eye movement is greater than their head movement in the vertical direction.
This has a direct connection to accommodation. Think of the student who sits at a desk or the office worker who stares at a computer screen all day. The primary direction of eye movement in these scenarios is likely to include looking up and down from the board (for the student) or looking up and down from the computer (for the office worker). Both are vertical motions that incorporate near-to-far movement requiring accommodation.
In addition to this phenomenon, cognitive demand has been shown to influence accommodation, so much so that increased difficulty of near work—in addition to the working distance itself—can increase a patient’s accommodative effort.2,3 In several more recent studies, small changes in against-the-rule astigmatism have been shown to occur with changing accommodation.4-8 It has been shown that children who begin school with low amounts of against-the-rule astigmatism tend to show myopia in later years; Dr. Martin Birnbaum put it like this: “The organism grows along the line of stress to reduce stress.”2,9 Given the current increase in myopia that we are seeing across the board, it behooves us to do whatever we can to preclude the onset of preventable disease from occurring.
 |
|
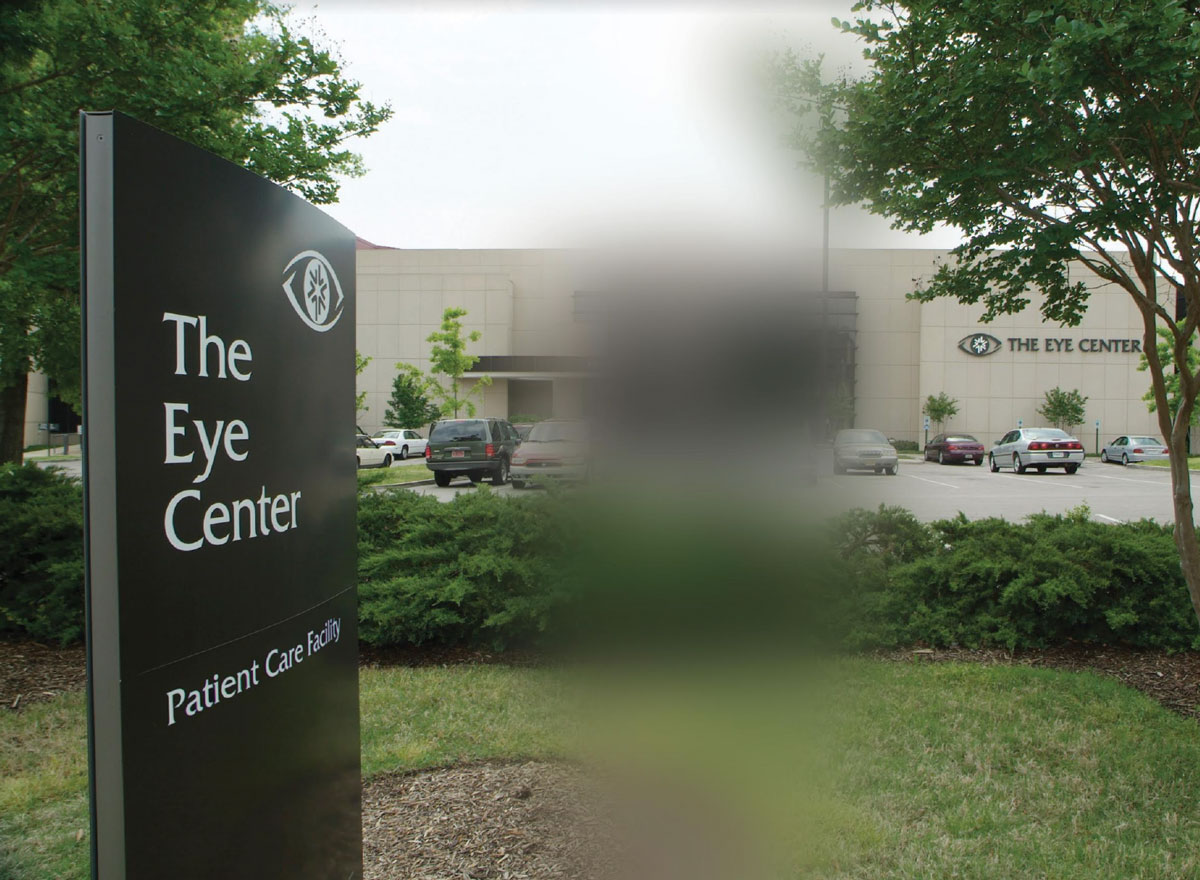
Simulation of significant cylindrical blur. Photo: Phillip Tribble, Southern College of Optometry. Click image to enlarge. |
So, how does this relate to prescribing? My general rule for low amounts of cylinder that appear in the refraction is this: the patient has to prove to me that it’s real (that is, constant) and that they really need it. I can’t recall the last time I actually prescribed -0.25 cyl; most -0.50 and many -0.75 against-the-rule cyls can be eliminated with no decrease in the patient’s acuity or function. Let me give a few examples:
Patient 1. An 18-year-old female showed retinoscopic findings of -2.50 DS OD and -1.75 DS OS. Manifest refraction showed -2.50 -0.50x110 OD and -2.50 -0.25x090 OS. Her best-corrected acuity was 20/20 with the retinoscopy, however. We opted to cut the cyl and go with a final Rx of -2.00 DS OU, through which she was still able to achieve 20/20 OD and OS. Accommodative findings in this case were mildly reduced with the manifest, but they were normal with the final Rx. There was no reason to include the additional cylindrical portion here.
Patient 2. A 16-year-old patient came in with unaided visual acuities of 20/30- OD and OS at distance and 20/200 OD and OS at 40cm. Her near point of convergence was quite reduced, to 11cm OD and 15cm OS, and her accommodative amplitudes were also low at 8.00D OD and OS. Retinoscopy revealed +0.50-0.50x090 OD and OS, but she was still able to achieve 20/20 in each eye with +0.50 spheres at both distance and near. Clearly, the against-the-rule cylinder was not necessary in her final Rx. She was asked to return for further binocular assessment.
Patient 3. A 16-year-old male presented with normal entering acuities (20/20 OD and OS at distance and 20/15 OD and OS at near) but reduced stereo of 100 sec, accommodative amplitude of only 6.00D OD and OS and low positive relative accommodation (NRA/PRA was +2.50/-0.75). Interestingly, his retinoscopy was plano -0.25x180 OD and plano -0.50x090 OS. Upon refraction, he took nothing (plano OD and OS) and was able to read 20/20 with ease. The small cylinders here reflected both accommodative and binocular instability. In this case, we deferred any Rx at all and enrolled him into a vision therapy program. As we begin therapy, we will consider +0.50 DS OU at near.
Patient 4. Lest you think that this phenomenon is isolated to pediatric patients, this case involved a 26-year-old who spent considerable time on the computer during the workday. His entering acuities were 20/20 OD and OS at distance but were reduced to 20/30 OD and OS at near. He showed retinoscopic findings of -0.50 -0.25x085 OD and -0.50 -0.50x100 OS, through which he could see 20/20—but he could do that unaided. Upon refraction, he kept the -0.50 spherical component in each eye, but his cylinder portion increased to -0.50x090 OD (no change in OS). Accommodative amplitudes and PRA were reduced (8.00D OD and OS and -1.25, respectively), and his MEM retinoscopy was +1.50. We performed a second retinoscopy following dilation, which showed +0.75 OD and +1.00 OS—with no remaining cylinder. He was ultimately prescribed +0.50 DS OU for all near work and asked to return for follow-up care (and possible vision therapy referral).
These cases illustrate how transient against-the-rule cylinder can creep into refractive findings. If we look closely, we can often see reduced or otherwise abnormal accommodative findings that accompany these cyls, but we have to look for them. Given the tendency for early astigmatism to lead to myopia, if we can avoid prescribing such cylinder, we can potentially prevent or slow down the onset of myopia. Your patients won’t be bothered by the lack of cyl in their glasses (they may not even notice either), but they will certainly appreciate not starting down the myopic path. You will be doing them a huge favor!
Dr. Taub is a professor, chief of the Vision Therapy and Rehabilitation service and co-supervisor of the Vision Therapy and Pediatrics residency at Southern College of Optometry (SCO) in Memphis. He specializes in vision therapy, pediatrics and brain injury. Dr. Schnell is an associate professor at SCO and teaches courses on ocular motility and vision therapy. She works in the pediatric and vision therapy clinics and is co-supervisor of the Vision Therapy and Pediatrics residency. Her clinical interests include infant and toddler eye care, vision therapy, visual development and the treatment and management of special populations. They have no financial interests to disclose.
1. Forrest EB. Stress and Vision. Santa Ana, CA: Optometric Extension Program, 1988. 2. Birnbaum M. Optometric Management of Nearpoint Vision Disorders. Butterworth-Heinemann, 1993. 3. Hynes NJ, Cufflin MP, Hampson KM, Mallen EAH. Cognitive demand and accommodative microfluctuations. Vision. 2018;2(36):1-11. 4. Bannon RE. A study of astigmatism at the near point with special reference to astigmatic accommodation. Am J Optom Arch Am Acad Optom. 1946;23:53-75. 5. Tsukamoto M, Nakajima T, Nishino J, et al. Accommodation causes with-the-rule astigmatism in emmetropes. Optom Vis Sci. 2000;77:150-5. 6. Ukai K, Ichihashi Y. Changes in ocular astigmatism over the whole range of accommodation. Optom Vis Sci. 1991;68:813-8. 7. Liu T, Thibos LN. Variation of axial and oblique astigmatism with accommodation across the visual field. J Vis. 2017;17:24. 8. Mutti DO, Enlow NL, Mitchell GL. Accommodation and induced with-the-rule astigmatism in emmetropes. Optom Vis Sci. 2001;78:6-7. 9. Hirsch MJ. Predictability of refraction at age 14 on the basis of testing at age 6—interim report from the Ojai longitudinal study of refraction. Am J Optom Arch Am Acad Optom. 1964;41(10):567-73. |

